Treatment options for Parkinson’s disease
Last updated Feb. 21, 2025, by Marisa Wexler, MS

There is no cure for Parkinson’s disease and, currently, no disease-modifying treatment can slow, stop, or reverse the progression of the neurodegenerative disorder. However, a wide range of treatments are available that can help to ease disease symptoms and make living with Parkinson’s more manageable.
Different medications are prescribed for motor versus nonmotor symptoms. While Parkinson’s mostly affects movement and balance, other disease-related problems such as dementia, sleep disturbances, mental health issues, and fatigue, may also require treatment.
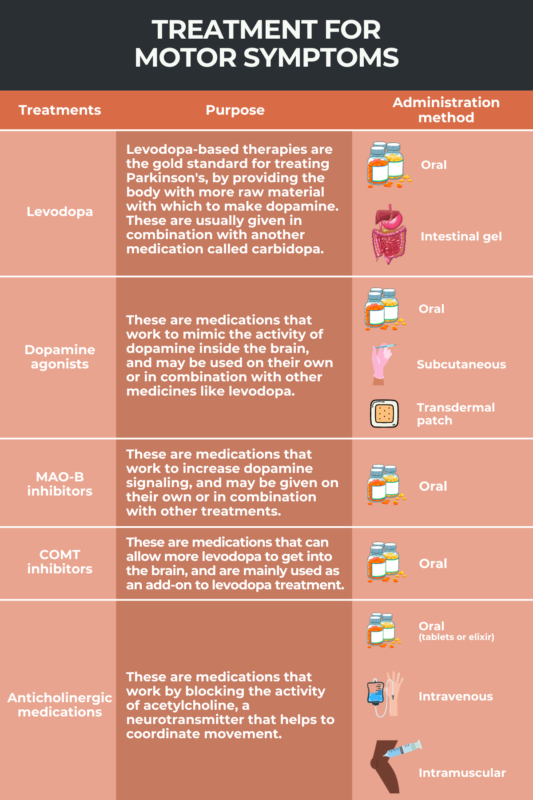
Treatments for motor symptoms
Parkinson’s primarily is defined by motor symptoms that include tremor, rigidity, trouble with balance, and slowed movements (bradykinesia).
Such problems are caused by reduced dopamine signaling. Dopamine is a neurotransmitter, a chemical that some specialized nerve cells use to communicate with each other and with the rest of the body. Signaling with dopamine is critical for controlling movement.
In Parkinson’s, dopamine-producing cells in the brain progressively die off, causing a drop in dopamine signaling that ultimately gives rise to the disease’s motor symptoms.
Several types of medications can be used to treat motor symptoms in Parkinson’s. These treatments mainly work by boosting dopamine signaling in the brain, or by altering the activity of other neurotransmitters that help control movement. Motor symptom treatments include:
- levodopa and its derivatives
- dopamine agonists
- MAO-B inhibitors
- COMT inhibitors
- anticholinergic medications.
Surgical treatments — particularly deep brain stimulation or DBS, which works to deliver electrical stimulation to activate specific regions of the brain — also may be used to help ease some motor symptoms of Parkinson’s.
Levodopa
Levodopa is widely considered the gold standard for treating Parkinson’s disease, as it usually is the most effective treatment for easing motor symptoms. In fact, seeing if a patient’s symptoms ease in response to treatment with levodopa is a test commonly used to help diagnose Parkinson’s.
The therapy has been used to treat Parkinson’s since the 1960s, and in the modern era, virtually everyone with Parkinson’s will be prescribed levodopa at some point.
Also known as L-DOPA, levodopa contains a molecule that cells in the body can use to make dopamine. The treatment basically works by giving the body more raw material with which to make dopamine, thereby boosting dopamine levels.
Levodopa often is given in combination with carbidopa, a medication that stops cells outside of the brain from using levodopa to make dopamine. This allows more levodopa to get into the brain, where it’s needed to ease Parkinson’s symptoms.
Dosages and formulations
Most formulations of levodopa are taken by mouth one or more times each day. Levodopa’s specific dosage and frequency of daily dosing varies widely, and generally is tailored for the individual based on what’s needed to relieve symptoms.
Approved oral formulations of levodopa include:
- Sinemet (carbidopa and levodopa)
- Rytary (carbidopa and levodopa)
- Stalevo (carbidopa, levodopa, and entacapone)
- Crexont (carbidopa and levodopa).
Other formulations of levodopa also exist. Duopa (carbidopa and levodopa), sold as Duodopa outside the U.S., is administered via a tube surgically inserted into the intestine. Vyalev, a soluble formulation of foscarbidopa and foslevodopa, is administered continuously and directly under the skin, where it can be absorbed into the bloodstream.
Over time, people with Parkinson’s typically will require higher and more frequent doses of levodopa to achieve symptom control. This is because as Parkinson’s progresses over time, more dopamine-making brain cells are lost so that fewer cells are available to convert levodopa into dopamine.
Side effects and off periods
Common side effects of levodopa include:
- nausea and vomiting
- decreased appetite
- lightheadedness
- low blood pressure
- confusion and hallucinations.
Sleepiness or impulsivity also can occur as side effects of levodopa, though these are less common.
Long-term treatment with levodopa commonly can cause dyskinesia, a side effect characterized by sudden, uncontrolled movements. It’s estimated that up to 30% of patients will develop dyskinesia after a few years on levodopa.
Formulations of amantadine, a therapy that works by blocking a brain signaling molecule called glutamate, may be used to help ease levodopa-induced dyskinesia. These medications include Gocovri and Osmolex ER.
It’s also common for people on long-term levodopa to experience periods in between doses where symptoms are not fully controlled. These are referred to as off periods, or off time — meanwhile, periods of time where symptoms are well controlled are called on periods.
There are a few Parkinson’s disease treatments approved to help control symptoms during off periods, including:
- Inbrija, an inhaled formulation of levodopa
- Apokyn (apomorphine), a dopamine agonist given by subcutaneous or under-the-skin injection
- Nourianz (istradefylline), an oral therapy that works by blocking A2A receptors in the brain
- amantadine formulations, including Gocovri and Osmolex ER, that also are approved for off episodes.
Dopamine agonists
Dopamine agonists are medications that work to mimic the activity of dopamine inside the brain. These therapies usually are less effective than levodopa for easing Parkinson’s motor symptoms, but they also are less likely to cause dyskinesia.
Used on their own or in combination with other medicines, such as levodopa, certain dopamine agonists may help to control motor symptoms. Approved dopamine agonists include:
- Mirapex (pramipexole), an oral therapy taken one or more times per day
- Apokyn (apomorphine), given as a subcutaneous injection
- Ropinirole, an oral medicine usually taken three times daily
- Neupro (rotigotine transdermal system), administered as a patch worn on the skin throughout the day
- Onapgo (apomorphine hydrochloride), delivered as a continuous subcutaneous infusion.
Common side effects of dopamine agonists include:
- sleepiness or sudden sleep attacks
- low blood pressure
- lightheadedness
- confusion or hallucinations
- leg swelling and discoloration.
As many as 40% of people treated with dopamine agonists will experience problems with impulse control, which can result in atypical compulsive behaviors like uncontrolled shopping, gambling, eating, and sexual urges. Further, while dyskinesia is less common with dopamine agonists than is levodopa, dopamine agonists still can cause dyskinesia in some instances.
Among people who stop taking dopamine agonists, as many as 20% will experience withdrawal symptoms, such as anxiety, panic attacks, irritability, or drug cravings.
MAO-B inhibitors
Monoamine oxidase-B, known as MAO-B, is an enzyme that normally works to break down dopamine in the brain. MAO-B inhibitors work to block this enzyme, thereby increasing dopamine signaling. These medicines may be given on their own or in combination with other treatments like levodopa.
Like dopamine agonists, MAO-B inhibitors usually are not as effective as levodopa for controlling Parkinson’s motor symptoms. But they are less likely to cause dyskinesia.
Approved MAO-B inhibitors include:
- Azilect (rasagiline), a once-daily oral therapy
- Eldepryl (selegiline), a twice-daily oral medication
- Zelapar (selegiline), a once-daily therapy that dissolves in the mouth
- Xadago (safinamide), an oral therapy used as an add-on to levodopa treatment.
Common side effects of MAO-B inhibitors include:
- nausea
- dry mouth
- lightheadedness
- constipation
- confusion or hallucinations.
COMT inhibitors
Short for catechol-O-methyl transferase, COMT is an enzyme that has the ability to deactivate levodopa before it enters the brain. COMT inhibitors, which block this enzyme, can allow more levodopa to get into the brain, where it’s most needed with Parkinson’s.
These therapies mainly are used as an add-on to levodopa treatment in people for whom levodopa alone is not sufficient to control symptoms throughout the day.
Approved COMT inhibitors include:
- Comtan (entacapone), an oral therapy taken with each levodopa dose
- Tasmar (tolcapone), taken by mouth three times daily
- Ongentys (opicapone), a once-daily oral medicine
- Stalevo, a combination therapy containing levodopa/carbidopa alongside the COMT inhibitor entacapone.
Common side effects of COMT inhibitors include:
- diarrhea
- red or brownish urine
- confusion or hallucinations
- worsening of dyskinesia and other levodopa-related side effects.
Anticholinergic medications
Anticholinergic medications are a group of treatments that work by blocking the activity of acetylcholine, a neurotransmitter that, like dopamine, helps to coordinate movements.
Such therapies can help to reduce tremor, and also may lessen the painful cramping, called dystonia, that’s associated with levodopa wearing off. Anticholinergic therapies generally are not very effective for other motor symptoms of Parkinson’s.
Two anticholinergic medications are approved to treat Parkinson’s, and both are taken orally a few times each day. These include:
Among the common side effects of anticholinergic medicines are:
- confusion or hallucinations
- problems with short-term memory
- dry mouth
- blurry vision
- difficulty urinating.
Because they frequently can cause side effects that impair cognition, anticholinergic medicines usually are used only in younger people without any underlying cognitive problems.
Surgery
Deep brain stimulation, known as DBS, is a surgical treatment that can be used to control motor symptoms. In DBS, one or more wires, called leads, are implanted into the brain. The leads connect out to a small electrical generator, called a neurostimulator, that is implanted in the chest, a bit like a pacemaker.
The implanted DBS device is able to deliver gentle electrical stimulation to specific brain regions. In doing so, this type of therapy aims to activate or interrupt the activity of specific parts of the brain so as to ease motor symptoms.
The surgery to implant a DBS device is an invasive process that usually requires additional monitoring before and after the procedure. Once the device is implanted, there’s usually a few weeks to allow the patient to heal, and then a doctor will work with the patient to program the device to generate specific patterns of electrical stimulation. Stimulation patterns that are most effective will vary from person to person, and there’s typically a process of trial and error to find the specific combination of settings that most helps any one person.
Among people with Parkinson’s disease, DBS is generally most helpful for patients with tremor that doesn’t respond to other treatment, or individuals who experience severe motor fluctuations and dyskinesia associated with other therapies wearing off. DBS also may be used to help control symptoms if medications cause unacceptable side effects.
Other surgical procedures
In addition to DBS, other surgical procedures may be used to help control Parkinson’s motor symptoms, though these are much less common than DBS.
A procedure called focused ultrasound is approved in the U.S. to treat people with Parkinson’s who have tremor that does not respond well to available medications. This procedure uses sound waves to destroy specific areas of the brain that are connected to tremor.
Procedures such as thalamotomy, pallidotomy, or subthalamotomy may be used in rare situations to help manage Parkinson’s disease. In all of these procedures, surgery is used to destroy a lesion, a small part of the brain, with the aim of easing symptoms. Because these procedures are by nature highly invasive, they are rarely done in the modern day, but may be used in certain specific instances.
Treatments for nonmotor symptoms
A wide array of different therapies are available to help manage the nonmotor symptoms of Parkinson’s. In most cases, treatments used for nonmotor problems are the same ones used to control these symptoms when they occur in people who don’t have Parkinson’s disease.
Specific nonmotor symptom treatments usually are targeted to the particular issue that’s affecting the patient.
- For dementia, Exelon (rivastigmine) is an approved treatment available in oral and skin patch formulations. The approved therapy is used, as it is in the general population, to ease the effects of dementia in people with Parkinson’s disease. Some treatments that are approved for dementia in Alzheimer’s, particularly donepezil and galantamine, also may help to manage dementia in Parkinson’s patients.
- For depression and anxiety, treatments for those with Parkinson’s generally are similar in nature to strategies used for other people with these conditions. Specifically, the treatment of mental health issues in Parkinson’s may include antidepressants and anti-anxiety medications.
- For psychosis (hallucinations and/or delusions), the first step in treating Parkinson’s patients typically is to adjust the dosage of medications that may contribute to symptom worsening. If additional treatment is needed to manage psychosis in people with Parkinson’s, Nuplazid (pimavanserin) is currently the only medication approved in the U.S to treat hallucinations and delusions associated with Parkinson’s disease psychosis.
- For sleep problems, treatment is dependent on the specific issue. For Parkinson’s patients with REM sleep behavior disorder, a condition in which an individual violently acts out dreams, supplements of melatonin or the sedative clonazepam may be used. Sedatives also can be given to help Parkinson’s patients with insomnia, while stimulants may be prescribed to help individuals with daytime sleepiness.
- For orthostatic hypertension, which is a drop in blood pressure upon standing, treatments may include Northera (droxidopa), midodrine, or fludrocortisone. Each of these medications can treat lightheadedness or fainting among Parkinson’s patients.
- For constipation, a variety of laxatives and prokinetics, which are medicines that prompt movement of the bowels, are commonly used in people with Parkinson’s. These medications, similar to what are used in the general population, can help manage constipation issues among patients.
- For excessive drooling, treatment for those with Parkinson’s may include formulations of botulinum toxin such as Myobloc (rimabotulinumtoxinB). Other therapies, like glycopyrrolate or sublingual or under-the-tongue atropine, also may be used to manage drooling in patients.
- For pseudobulbar affect, which manifests as uncontrolled crying or laughing, the only therapy specifically approved in the U.S. is Nuedexta (dextromethorphan HBr and quinidine sulfate). Antidepressants also may help manage this symptom in Parkinson’s patients.
Supportive therapies
In addition to medications and surgeries, a range of supportive therapies may help people with Parkinson’s to manage their symptoms and make it easier to navigate life with the disease.
Exercise
There is robust evidence that getting regular physical exercise is beneficial for people with Parkinson’s disease. Studies indicate that exercise can help patients maintain mobility, improve balance, ease motor symptoms, and even help to ease nonmotor symptoms like depression or constipation.
The Parkinson’s Foundation has published a set of recommendations on exercise for Parkinson’s patients. These suggest that patients should try to get:
- aerobic exercise, defined as moderate to vigorous activity that raises the heart rate, three times per week, for at least 30 minutes per session
- strength training, such as using weights or resistance bands, two to three times per week
- balance and agility training, like yoga, dance, or boxing, two to three times each week with additional training on a daily basis
- stretching done at least two to three days per week.
Physiotherapy
Also called physical therapy, physiotherapy is a rehabilitative technique that aims to help strengthen the body and improve flexibility. Its ultimate goal is improving and stabilizing motor function.
A physical therapist can help guide patients through exercises during sessions, and also can work with people with Parkinson’s to help establish an exercise routine that works for them.
Physiotherapy for Parkinson’s patients can help to ease the severity of motor symptoms, reduce the risk of problems like falls, and make it easier to move around.
Occupational therapy
Occupational therapy is a rehabilitation technique that aims to create strategies that make day-to-day life with Parkinson’s easier. In Parkinson’s disease, occupational therapy is used to help patients continue with their daily tasks as the disease progresses. An occupational therapist will work with a patient to address specific challenges that the person is facing, such as finding new ways to perform activities that are harder to do with Parkinson’s.
Speech therapy
Many people with Parkinson’s experience difficulties with speech, especially as the disease progresses. Speech therapy aims to help improve a person’s speaking ability and to find other strategies to make it easier for patients to communicate. In addition to helping improve speech, this type of therapy also may help to improve swallowing abilities.
Diet and nutrition
For anyone, maintaining a well-balanced diet and getting enough nutrition is an important part of overall good health. While no specific diet is recommended for people with Parkinson’s, it’s generally suggested that patients try to eat a diet similar to what’s recommended for the general population: plenty of whole grains, vegetables, fruits, and protein-rich foods, while limiting excess sugar, fats, or processed foods.
Meditation
Meditation and mindfulness are techniques that aim to calm the body and allow individuals to focus on their own emotional and physical state. Studies have suggested that these techniques can help to ease Parkinson’s symptoms and improve patients’ experiences in day-to-day life.
The Parkinson’s Foundation has published a mindfulness toolkit that’s available online. It includes short instructional videos to guide patients through introductory mindfulness and meditation techniques specific to those with Parkinson’s disease.
Medical marijuana
Marijuana or cannabis, a plant that contains a variety of biologically active compounds, has been used by humans for millennia for recreational as well as medicinal purposes. In recent years, there has been a surge of interest in the potential benefits of medical marijuana for many conditions, including Parkinson’s disease.
Despite the interest, however, no evidence to date conclusively supports medical marijuana being beneficial in Parkinson’s disease. Although some data indicate marijuana can help to ease anxiety, promote sleep, reduce nausea, and lessen pain for Parkinson’s patients, these potential benefits remain unproven. Moreover, most studies conducted to date have been small and prone to biases.
Besides its potential benefits, using marijuana can carry risks, such as problems with cognition, changes in mood, and difficulties with balance. It’s strongly advised that Parkinson’s patients who are interested in trying medical marijuana should talk with their healthcare provider about whether and how they can safely try marijuana.
Parkinson’s News Today is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or another qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recent Posts
- Breathing CO2 activates brain cleanup signals in new Parkinson’s study
- Guest Voice: DBS surgery transformed my life with early-onset Parkinson’s
- Smartphone app helps Parkinson’s patients map daily symptoms
- Spinal stimulation found safe, shows mixed benefits in small study
- SCAN brain network may offer new treatment target in Parkinson’s
FAQs about Parkinson’s disease treatments
There is no cure for Parkinson’s disease, and there are no available treatments that have been proven to slow or stop the progression of the neurodegenerative disorder. However, a range of medications and other treatments are available that can help to ease the symptoms of Parkinson’s and make living with the disease more manageable.
Although there aren’t any medications that can slow or stop the progression of Parkinson’s disease, a variety of medicines are available that can help to ease disease symptoms.
Levodopa and its derivatives are generally the most effective treatment for controlling the motor symptoms of Parkinson’s, though these medicines typically become less effective as the disease progresses. Their long-term use also can cause unpleasant side effects such as dyskinesia (uncontrolled movements). Other medications such as dopamine agonists or MAO-B inhibitors usually aren’t as effective for easing motor symptoms, but may be used on their own or in combination with levodopa to attain optimal symptom management with minimal side effects.
All of the available treatments for Parkinson’s work to ease the disease’s symptoms. In addition to Parkinson’s-specific therapies that can help to control motor symptoms, a wide range of symptom-specific medicines may be helpful for dealing with nonmotor complications of the disease.
Every person with Parkinson’s disease has a unique experience with disease symptoms and treatment responses. Finding the ideal treatment for any one person often is a process that involves some trial and error — trying out different available therapies to find one or more treatments that are effective for controlling symptoms without causing unbearable side effects.