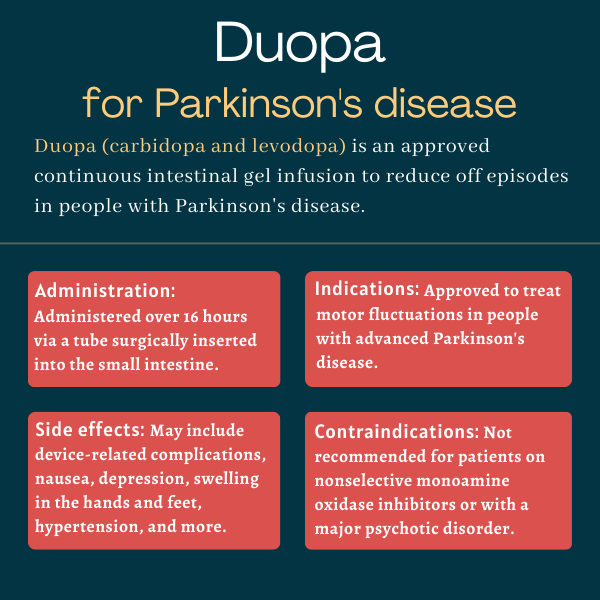
Duopa (carbidopa and levodopa) for Parkinson’s disease
What is Duopa for Parkinson’s disease?
Duopa is an approved intestinal gel formulation of levodopa and carbidopa that is used to treat motor fluctuations in patients with advanced Parkinson’s disease. The therapy is administered via a tube surgically inserted into the small intestine, where levodopa is mostly absorbed.
The gel is continuously delivered over an extended period of time, typically about 16 hours, which helps to maintain stable levodopa levels for longer periods. This method of administration has been shown in clinical trials to reduce off episodes, or periods when a medication wears off and motor symptoms return. It also was found to reduce the number of levodopa-containing pills required by patients.
In addition to its U.S. approval, Duopa, marketed by AbbVie, is approved in several other countries, where is it sold under the brand name Duodopa. The drug is not yet available in generic form.
Therapy snapshot
| Brand Name: | Duopa |
| Chemical Name: | Carbidopa and levodopa |
| Usage: | Used to treat motor fluctuations in advanced Parkinson’s disease |
| Administration: | Continuous delivery as an intestinal gel |
How does Duopa work?
Parkinson’s disease is characterized by the loss of the neurotransmitter dopamine — a chemical messenger that allows for the transmission of electric signals between nerve cells and from the brain to various muscles in the body.
Dopamine cannot be directly administered to patients because it cannot cross the blood-brain barrier, a semipermeable membrane that protects the brain and spinal cord from potential threats, like viruses and large molecules, circulating in the bloodstream.
Levodopa is the chemical building block from which dopamine is synthesized in the body. It can cross the blood-brain barrier easily and be converted to dopamine in the brain, easing Parkinson’s symptoms such as muscle stiffness and involuntary movements.
Carbidopa is an agent that helps prevent the breakdown of levodopa outside the nervous system, so more of it is available to make dopamine in the brain. This reduces the amount of levodopa that needs to be administered, helping to limit certain side effects of levodopa treatment.
Duopa is given to patients as a gel suspension through a tube surgically inserted into the stomach and through the small intestine. As such, its administration bypasses the stomach and allows levodopa to be more quickly absorbed.
A pump helps to deliver the required dosage continuously through the tube, ensuring a steady concentration of the therapy is available in the blood over long periods.
Who can take Duopa?
Duopa was approved by the U.S. Food and Drug Administration in 2015 to treat motor fluctuations in patients with advanced Parkinson’s disease.
The therapy had been previously approved in the European Union in 2005. It’s sold there under the brand name Duodopa for a similar indication. As of 2015, the therapy was approved in more than 40 countries, according to AbbVie.
Who should not take Duopa?
Duopa is not recommended for people also receiving treatment with a nonselective monoamine oxidase (MAO) inhibitor — an antidepressant medication — or who have taken a nonselective MAO inhibitor within two weeks. Using the two medications together may lead to hypertension, or an increase in blood pressure.
The treatment also is generally not recommended for patients with a major psychotic disorder, as it can increase the risk of a psychosis exacerbation.
How is Duopa administered in Parkinson’s?
Duopa is available as an intestinal gel suspension that comes in single-use cassettes containing 4.63 milligrams (mg) carbidopa and 20 mg levodopa per milliliter (mL). Each cassette contains approximately 100 mL of suspension.
The cassette attaches to a pump device that administers the medicine through a tube directly into the small intestine over a 16-hour infusion period. This procedure requires a specialist to make a small hole in the stomach wall to place the medication delivery port, called a percutaneous endoscopic gastrostomy with jejunal tube (or PEG-J). After that, a healthcare provider connects the portable pump that delivers levodopa continuously.
Short-term, temporary administration of Duopa — before the placement of the PEG-J tube — may be done with the use of a nasojejunal tube. That tube is passed through the nose and into the small intestine. Such usage allows healthcare providers to observe a patient’s clinical response to the medication.
The pump delivers Duopa in three steps: a morning dose, in which a large daily dose of the medication is given over 10-30 minutes; a continuous dose, where Duopa is steadily delivered throughout the day; and extra doses, in which a small dose of Duopa is given as needed during the day.
Before treatment with Duopa, patients should convert from all other forms of levodopa to oral immediate-release carbidopa-levodopa tablets. Patients should remain on a stable dose of their other Parkinson’s medications.
Dosage
The maximum recommended daily dose of Duopa is 2,000 mg of levodopa (or one cassette per day), administered over 16 hours.
The starting dose of Duopa is determined by converting the amount of oral immediate-release levodopa taken by the patient on the previous day. Then, daily doses of Duopa can be titrated (adjusted upward) as needed, based on individual clinical responses and tolerability, until a stable daily dose is maintained. Over time, and depending on a patient’s level of activity and disease progression, additional dose adjustments may be necessary.
If persistent off periods — when symptoms are not fully controlled between doses — occur during the daily infusion, it may be necessary to increase the dosage or use an extra dose. That extra dose should be set at 20 mg of levodopa when initiating Duopa treatment, and can be adjusted in 4 mg increments. The extra dose frequency should be limited to one extra dose every two hours. However, administering frequent extra doses may cause or worsen dyskinesias, or uncontrolled movements.
If dyskinesia or adverse reactions occur due to Duopa treatment, it may be necessary to decrease the dosage or stop the infusion until the adverse reactions disappear.
If Duopa infusion is stopped for less than two hours (such as to shower, swim, or a for short medical procedure), patients may require an extra dose before disconnecting the pump from the tube. If the interruption lasts more than two hours patients should call their healthcare provider and take oral carbidopa-levodopa as prescribed until they are able to restart Duopa infusion.
Storage and maintenence
Duopa cassettes are stored in the freezer and thawed in the refrigerator. The cassettes should be taken from the refrigerator about 20 minutes before dosing to reach room temperature, at which point they can be connected to the pump and then to the stomach tube.
At the end of the daily infusion, patients should disconnect the pump from the delivery port, flush it with drinking water using a syringe, and take their nighttime dose of oral immediate-release carbidopa-levodopa tablets as prescribed by their doctors.
Duopa requires patients wear the portable pump in the belt region. Duopa carrying cases come in multiple different styles, including a fitted belt, a lightweight vest, and a cross-body pack, and patients can chose whatever works best for them.
Because it decreases the absorption of levodopa, a high-protein diet should be avoided in people taking Duopa. Patients taking iron salts or multivitamins that contain iron salts also should take Duopa with caution, as the supplements may reduce the medication’s availability and its ability to control symptoms.
Duopa in clinical trials
Duopa’s approval was based on data from two identically designed Phase 3 clinical trials — NCT00357994 and NCT00660387 — that were later merged into one single trial before enrollment was complete.
A total of 71 patients with advanced Parkinson’s were enrolled. All were experiencing persistent motor fluctuations (off periods) despite being on optimized treatment for the condition. Participants were randomly assigned to receive either Duopa or immediate-release carbidopa-levodopa capsules (25/100 mg) for three months.
In the first four weeks, patients were allowed to adjust their dose, based on investigator judgment, to reach optimal symptom control and a reduction in off periods. At the end of the three months, the mean levodopa dose was 1,117 mg/day in the Duopa group and 1,351 mg/day in the oral immediate-release carbidopa-levodopa group.
The trial’s main goal was to assess changes in daily off periods from the study start to the end of the trial. Secondary measures included changes on various scales: in on time without troublesome dyskinesia; in measures of quality of life; and in the second and third parts of the standard Unified Parkinson’s Disease Rating Scale (UPDRS). The second part of UPDRS assesses a patient’s ability to perform daily activities, whereas the third part measures motor symptoms.
In all, 66 patients — about 85% — completed the trial. After three months, Duopa had reduced the daily mean off time by four hours, while total off periods were lowered by 2.1 hours with the oral capsules. This translated in a significant 1.9-hour greater reduction in off time with Duopa.
The treatment also improved mean on time without troublesome dyskinesia by about four hours compared with the study’s start — also a 1.9-hour improvement compared with patients given immediate-release carbidopa-levodopa. Significant improvements also were observed in the ability to perform daily activities and in some quality of life measures, although no group differences were observed in motor symptoms.
DYSCOVER
After Duopa’s approval, AbbVie launched another Phase 3 trial to investigate the treatment’s effect on dyskinesia. Called DYSCOVER (NCT02799381), the study evaluated Duopa in 63 patients with advanced Parkinson’s who were experiencing persistent motor fluctuations and uncontrolled dyskinesia despite being on optimal Parkinson’s treatment.
The participants were randomly assigned to continue their optimal treatment regimen or to switch to treatment with Duopa for three months. Those who switched to the intestinal treatment were allowed to adjust their dose to obtain the optimal clinical response.
The main goal of this study was to measure treatment impact on dyskinesia, as assessed by the Unified Dyskinesia Rating Scale (UPDRS). Other measures included changes in on time without troublesome dyskinesia, off time, UPDRS Part 2 and 3 scores, and quality of life.
The trial met its main goal. Compared with optimal medication, which lowered dyskinesia by 2.33 points after three months, Duopa reduced dyskinesia scores by 17.37 points — a significant difference.
The intestinal gel also significantly increased mean on time without troublesome dyskinesia and reduced off periods. Additionally, Duopa improved quality of life measures, and significantly increased patients’ ability to perform activities of daily living and motor control. In most of these measures, significant benefits were observed as early as two weeks after treatment start.
DUOGLOBE
An observational study called DUOGLOBE (NCT02611713) evaluated Duopa’s safety and effectiveness over the long term (three years) in 213 adults with advanced Parkinson’s disease treated in a real-world setting. Participants came from 10 countries, including the U.S.
Interim data showed the treatment to be safe and effective in reducing motor and nonmotor symptoms and in improving quality of life over two years of use. A significant lessening in off time also was found, beginning three months after the start of treatment. Gastrointestinal complaints were among the most common adverse events, or side effects.
Common side effects of Duopa
The most common adverse reactions reported in Duopa clinical trials include:
- complications with device insertion
- nausea
- depression
- swelling (edema) in the hands and feet
- high blood pressure
- upper respiratory tract infections
- throat pain
- partial or complete collapse of the lung (atelectasis)
- irritation at the incision site.
Gastrointestinal complications
Gastrointestinal complications can occur when using a PEG-J or nasojejunal tube. These can have serious consequences, such as a need for surgery, or death. Patients should inform their healthcare provider if they experience any gastrointestinal symptoms while using Duopa.
Among the potential complications are abscess, accumulation of hairs or fibers in the stomach (bezoar), and implant site erosion or ulcer. Intestinal bleeding, decreased intestinal blood flow, and intestinal obstruction or perforation also can happen.
Falling asleep during daily activities
Some people on levodopa-based therapies have reported suddenly falling asleep during activities of daily living. Before initiating treatment with Duopa, healthcare providers should discuss with patients whether there are any factors for increased sleepiness, such as sleep disorders and other coprescribed sedating medications.
Patients should consider discontinuing treatment if severe cases of daytime sleepiness or episodes of falling asleep during daily activities occur. However, if the therapy is not stopped, driving and other activities where falling asleep unexpectedly can be dangerous should be stopped.
Low blood pressure upon standing
Duopa can cause low blood pressure that may result in dizziness, lightheadedness, or fainting when rising from a sitting or lying down position; this is known as orthostatic hypotension. Monitoring for this form of low blood pressure should be done for all patients, but especially for those starting Duopa or increasing their dose.
Hallucinations, psychosis, and impulse control
There is an increased risk for mental health problems, such as hallucinations (seeing or hearing things that are not real), confusion, and psychotic behavior in patients taking Duopa. Due to a risk of worsening psychosis, individuals with a major psychotic disorder should not be treated with this medication.
Patients taking Duopa also may experience impulse control problems, such as urges to gamble and eat, or increased sexual urges. Dose reductions or treatment discontinuation should be considered for patients experiencing impulse control disorders.
Depression and suicidal tendencies
Duopa-treated patients can develop depression or experience worsening of depression. Patients should pay close attention to any sudden changes in mood and behavior and contact their healthcare provider if they experience depression or suicidal thoughts.
High fever and confusion associated with rapid dose reductions
High fever, stiff muscles, changes in breathing and heartbeat, and confusion have been reported following rapid dose reductions or discontinuation of dopaminergic therapy. Individuals taking Duopa should avoid sudden discontinuation or rapid dose reductions of the medication. Those who decide to discontinue treatment should do so gradually to avoid these withdrawal symptoms.
Dyskinesia
Treatment with Duopa can cause or worsen dyskinesia — uncontrolled, involuntary movements — which can require a dosage reduction of either Duopa or other Parkinson’s medications.
Nerve damage
Before starting Duopa, patients should be assessed for signs and symptoms of peripheral neuropathy. These include progressive weakness and numbness or loss of sensation in the fingers or feet, due to nerve damage. Periodically monitoring patients for this complication also is recommended, especially in individuals with preexisting neuropathy or with medical conditions associated with it.
Heart problems and eye issues
There have been reports of heart rhythm abnormalities and heart attacks in patients taking carbidopa-levodopa treatment. Patients with glaucoma, a disease that can cause vision loss and blindness, also can experience increased pressure inside the eye. Anyone with glaucoma or a history of heart disease prescribed Duopa should be monitored closely for those complications.
Abnormal blood tests results
Abnormal lab test results have been seen in some patients treated with Duopa. Such results include increased levels of a marker of kidney damage known as urea nitrogen, and abnormal levels of creatine phosphokinase, a marker of heart, muscle, or brain damage. Use of the medication also may increase certain metabolites and lead to false positive results in some tests.
Use in pregnancy and breastfeeding
Duopa has not been well studied in patients who are pregnant or breastfeeding. Based on animal studies, the therapy may cause harm to a developing fetus.
Traces of levodopa also have been found in human breast milk. As such, caution should be used when administering Duopa to nursing patients. Levodopa also may inhibit lactation or milk production.
Patients who are or plan to become pregnant, and those who are nursing or plan to breastfeed, should discuss this issue with their healthcare providers and carefully weigh the potential benefits and risks of using the medication in these circumstances.
Parkinson’s News Today is strictly a news and information website about the disease. It does not provide medical advice, diagnosis or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or another qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recent Posts
- Navigating the effects of Parkinson’s disease on speech, part 3
- NIH consortium to explore gut-brain connection in Parkinson’s
- Researchers ID 3 genes linked to disease activity in Parkinson’s
- Tavapadon’s flexible dose eases symptoms in early Parkinson’s
- Potential diagnostic tool finds protein clumps in living cells
FAQs about Duopa
The U.S. Food and Drug Administration (FDA) approved Duopa in January 2015 for the treatment of motor fluctuations in people with advanced Parkinson’s disease. That FDA approval made Duopa the first treatment in the U.S. providing 16 continuous hours of carbidopa and levodopa for motor fluctuations in advanced Parkinson’s patients.
While animal studies suggest Duopa may cause harm to a developing fetus, the therapy has not been well studied in pregnant women. Patients who become or intend to become pregnant should always talk to their healthcare providers about the potential risks and benefits of taking Duopa during pregnancy.
Some patients on Duopa have reported sleepiness and suddenly falling asleep without warning during daily activities. Individuals starting treatment with Duopa should not drive and should avoid other potentially dangerous activities that might result in harm until they know how the medication affects them. If patients experience increased sleepiness or fall asleep without warning while taking this medication, they are advised to contact their healthcare team.
In the trials that supported Duopa’s approval, participants began seeing improvements as soon as two weeks after starting on the therapy. These advanced Parkinson’s disease patients experienced a reduction in off periods and improvements in other measures that became significantly more pronounced than with control medications. However, as each person is unique and responds differently to medications, patients are advised to discuss with their doctor how the therapy can help in their individual case.
There have been some reports of weight gain in people receiving Duopa, possibly due to the therapy’s potential to cause impulse control disorders, including compulsive eating. Hair loss also may occur with Duopa, although much less frequently. Those who experience any unanticipated effects of treatment should discuss them with their healthcare team.
Related Articles

 Fact-checked by
Fact-checked by