Parkinson’s disease symptoms
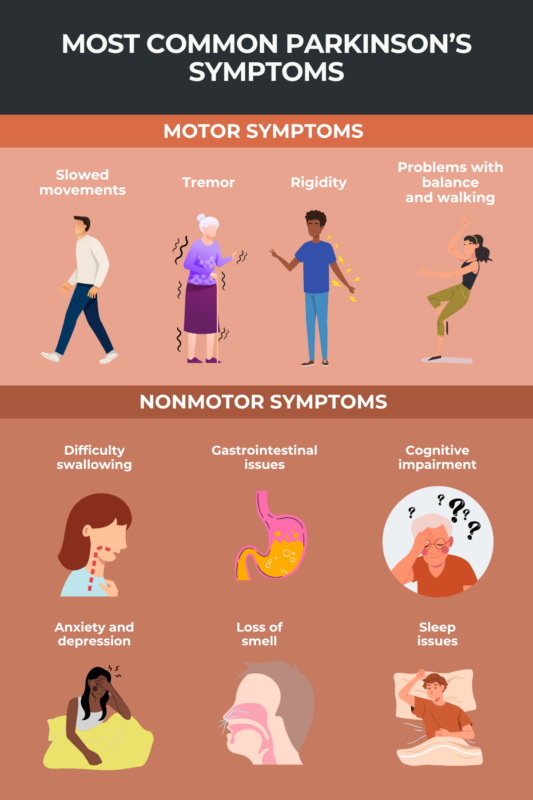
Parkinson’s disease can cause a wide array of symptoms. The disease is perhaps best known for how it affects movement and balance, creating problems with tremor, rigidity, and slowed movement. People with Parkinson’s can also experience nonmotor symptoms that may lead to problems with cognition, mental health, and sleeping.
Parkinson’s is a progressive disorder where symptoms usually start off very subtly, then gradually worsen with time. The disease affects every person differently, and not everyone will experience all the possible symptoms or progress at the same rate. With advances in treatment, most people with Parkinson’s, estimated at more than 10 million worldwide, are expected to have a normal or near-normal life expectancy.
Parkinson’s is caused by the loss of brain cells responsible for making a chemical messenger called dopamine. The lack of dopamine signaling is ultimately what gives rise to most symptoms of Parkinson’s disease.
Motor symptoms
Parkinson’s disease is characterized by changes in movement. The presence of these motor symptoms is critical for confirming a diagnosis of Parkinson’s.
Motor symptoms in Parkinson’s are commonly divided into four main categories:
- bradykinesia (slowed movements)
- tremor
- rigidity
- postural instability (problems with balance and walking difficulties).
Slowed movements
Bradykinesia, or abnormally slowed movements, is one of the disease’s core symptoms. In fact, based on current diagnostic criteria, a person can only be formally diagnosed with Parkinson’s if this symptom is present, alongside other motor symptoms such as tremor and rigidity.
Bradykinesia may manifest with changes in walking that cause a slow, shuffling gait or less swinging of the arms while walking. Patients may also experience more difficulty in starting movements, such as rising from a chair.
Parkinson’s bradykinesia can affect the hands, making it more difficult to perform activities that require a lot of dexterity and precise control of the fingers, such as buttoning a shirt, brushing teeth, cutting food, or opening packages. The face may be affected, leading to slowed blinking and less active facial expressions.
People who are experiencing bradykinesia often describe it as feeling similar to profound tiredness or abnormal muscle weakness.
Tremor
Tremor, or involuntary shaking, is one of the most well-known symptoms of Parkinson’s. Tremors make it harder to perform many activities that require fine motor coordination, such as shaving, writing, and getting dressed.
As one of the first early symptoms of Parkinson’s disease, tremor usually affects only one side of the body first, then spreads to affect both sides as the disease progresses.
The main type of tremor seen in people with Parkinson’s is known as a resting tremor. In this type of tremor, the shaking becomes most apparent when the person is not consciously moving their body, but during conscious movement, the tremor gets less intense or may seem to disappear entirely. For example, the hands may shake when the person is standing without moving their hands, then the shaking lessens when the person goes to pick something up.
Patients often experience a so-called “pill-rolling” tremor, which is characterized by hand movements that look as if the person is continually rolling a small object between the thumb and forefinger. They may also experience a supination and pronation tremor, where the palm flips up and down.
Tremor can also affect other body parts, including the mouth or legs. Some patients even report feeling an internal tremor, or an invisible shaking sensation in the abdomen or chest.
Although tremor is a well-known symptom of Parkinson’s and is present in most patients, as many as 1 in 5 people with the disease will not experience tremor. This symptom appears to be slightly less common in younger people with Parkinson’s.
Rigidity
Rigidity refers to muscles that are abnormally stiff and tight, limiting normal range of motion. This can make movements such as standing up more challenging, and contribute to reduced swinging of the arms while walking, reduced facial expressions, and balance problems.
Due to the combination of rigidity and bradykinesia, many people with Parkinson’s have abnormally small handwriting, referred to as micrographia. These motor symptoms can also cause vocal issues and problems with speech. Many people with Parkinson’s have an unusually soft and quiet speaking voice, referred to as hypophonia.
Rigidity can lead to pain and discomfort in affected muscles and make it harder to roll over in bed, hampering efforts to get comfortable and fall asleep.
When force is applied to help bend the rigid limb of someone with Parkinson’s, the muscles will often respond with short, jerky movements and pauses in between. This is often called “cogwheel” rigidity, as the movement resembles the way a gear moves.
Rigidity usually isn’t a prominent symptom in the earliest stages of Parkinson’s. However, virtually all patients will experience some rigidity as the disease progresses. Rigidity typically affects just one side of the body at first, then it can spread to other areas over time.
Problems with balance and walking
Difficulties with balance and walking affect most people with Parkinson’s, though these symptoms usually don’t develop until relatively late in the course of the disease.
Balance problems, also called postural instability, can increase the risk of falls, which can cause serious injury. Therefore, an important part of disease management for most patients is taking precautions to mitigate the risk of falls, including doing exercises to improve balance as well as removing tripping hazards from the environment.
People with Parkinson’s commonly experience changes in how they walk, often taking many small steps at a slower pace than normal. They also tend to have difficulty turning around (usually needing to take many small steps to do so), and to shuffle while they walk, with less movement in the arms and torso.
Freezing, or akinesia, is when a person is momentarily unable to move their muscles or limbs, and commonly occurs in patients when they start walking, or when faced with a doorway or passerby. Freezing may increase the risk of falls.
Medication side effects
Most people with Parkinson’s are treated with levodopa and its derivatives, which are therapies that can help the brain to produce more dopamine. While these treatments can be effective for managing Parkinson’s, their long-term use usually leads to dyskinesia, or erratic, uncontrolled movements.
Dyskinesia is not a symptom of Parkinson’s itself, but since most patients are treated with levodopa and related therapies, many of them experience dyskinesia. This side effect usually develops after patients have been on these medications for several years.
Other motor symptoms
In some patients, Parkinson’s causes other motor symptoms, including vision problems such as blurred vision or difficulty looking up, painful muscle cramps (dystonia), and difficulty maintaining an upright posture which can lead to stooping and abnormal curvature of the spine (scoliosis or kyphosis).
Nonmotor symptoms
While these nonmotor symptoms are not used to define a Parkinson’s diagnosis, they can cause substantial problems in day-to-day life.
Autonomic dysfunction
The autonomic nervous system is responsible for controlling involuntary bodily processes, such as regulating breathing, digestion, and blood pressure. People with Parkinson’s commonly experience autonomic dysfunction, where the autonomic nervous system is unable to properly regulate these involuntary processes. This can lead to symptoms including:
- difficulty swallowing (dysphagia)
- increased sweating (hyperhidrosis)
- excessive drooling (sialorrhea)
- orthostatic hypotension, where blood pressure suddenly drops when a person stands up, which can cause lightheadedness and, in severe instances, fainting
- gastrointestinal issues such as constipation or incontinence
- urinary issues such as needing to urinate frequently or feeling a strong sense of urgency to urinate
- problems with sexual performance and satisfaction such as erectile dysfunction or vaginal tightness.
Mood and cognitive changes
Issues with mental health and cognition affect many people with Parkinson’s and may include:
- depression
- anxiety
- apathy (loss of motivation)
- psychosis, which can include hallucinations (seeing, hearing, or otherwise sensing something that isn’t there) and/or delusions (fixed beliefs with no basis in reality)
- problems with decision-making and multitasking
- memory issues
- bradyphrenia (slowed thinking) or abulia (temporary inability to think or act).
People with Parkinson’s have a six times higher chance of developing dementia, where cognitive problems become severe enough that they cause issues in day-to-day life.
Sensory problems and skin issues
Many people with Parkinson’s experience changes in sensation such as:
- loss of smell (hyposmia)
- oily skin (seborrhea)
- tingling or burning sensations.
People with Parkinson’s are at increased risk of developing skin cancers such as melanoma.
Sleep issues
People with Parkinson’s often have trouble getting good sleep, due to issues like difficulty falling asleep and waking up frequently in the night or very early in the morning. Patients also commonly report feeling sleepy during the daytime, and may experience sudden attacks of sleepiness.
Another common disease complication is REM sleep behavior disorder, where a person will act out dreams by making noises and large, often violent, movements. (REM, or rapid eye movement, is the period of sleep where dreaming occurs).
Restless legs syndrome, where a person feels the need to move their legs due to uncontrolled discomfort, can affect people with Parkinson’s. This sensation typically is most problematic when a person is laying down or sitting, or trying to sleep.
Early signs
Although when symptoms appear and how quickly they progress varies for every patient, certain symptoms and signs are common in the early stages of Parkinson’s disease. These include:
- constipation
- REM sleep behavior disorder
- loss of smell
- depression
- fatigue
- tremor
- difficulty rising from a chair
- small, cramped handwriting
- weak voice
- reduced facial expression
- dizziness or fainting
- stooping or hunching over
- arms not swinging normally while walking.
Related conditions that cause Parkinson’s-like symptoms
Most symptoms of Parkinson’s disease are not unique to Parkinson’s and are also found in other conditions. One of the main challenges in diagnosing Parkinson’s is ruling out other disorders that can cause similar symptoms.
Some of the conditions that can cause Parkinson’s-like symptoms include:
- Essential tremor, a type of uncontrolled shaking, can affect the hands, arms, and voice. These tremors usually affect both sides of the body and are worse when a person is moving, unlike the tremors seen in Parkinson’s disease that typically start on one side of the body and are usually worse when the patient is at rest.
- Normal pressure hydrocephalus occurs when the fluid around the brain and spinal cord does not drain properly, putting abnormal pressure on the nervous system. It can cause Parkinson’s-like symptoms such as trouble walking, issues with urination, and cognitive difficulties.
- Corticobasal syndrome is characterized by Parkinson’s-like symptoms like stiffness and tremor, but also other symptoms such as uncontrolled movements and difficulty with language.
- Multiple system atrophy can cause many symptoms similar to those seen in Parkinson’s, but it’s characterized by more widespread damage in the nervous system, particularly in the autonomic nervous system that controls unconscious bodily functions.
- Progressive supranuclear palsy is another disorder that can appear similar to Parkinson’s but is marked by unique symptoms, including abnormal eye movements and a tendency to lean backward (whereas people with Parkinson’s usually stoop forward).
- Dementia with Lewy bodies also causes many symptoms similar to Parkinson’s, but these symptoms usually appear in a different order. In Parkinson’s, motor symptoms develop early on, whereas in dementia with Lewy bodies, cognitive problems are the first symptoms to appear.
Parkinson’s News Today is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or another qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recent Posts
- Navigating the effects of Parkinson’s disease on speech, part 3
- NIH consortium to explore gut-brain connection in Parkinson’s
- Researchers ID 3 genes linked to disease activity in Parkinson’s
- Tavapadon’s flexible dose eases symptoms in early Parkinson’s
- Potential diagnostic tool finds protein clumps in living cells
FAQs about Parkinson's disease symptoms
Like many other symptoms of Parkinson’s, tremor is caused by a lack of dopamine signaling. Dopamine is a chemical that nerves use to communicate with each other and the rest of the body. Parkinson’s is caused by the death and dysfunction of brain cells responsible for making dopamine.
Although Parkinson’s disease symptoms tend to worsen over time, how quickly these symptoms progress varies from patient to patient, and it’s currently difficult to make accurate predictions about the speed of disease progression.
While Parkinson’s symptoms tend to get progressively worse over time, symptom severity can vary from day to day and even from hour to hour. Symptoms that cause problems on one day may be less problematic the next. Medications to control symptoms may help to improve the experience of living with Parkinson’s disease, but no treatments are currently available that can slow or stop the overall progression of the disease.
Related Articles

 Fact-checked by
Fact-checked by