Benztropine mesylate for Parkinson’s disease
Last updated Feb. 16, 2024, by Marisa Wexler, MS

What is benztropine mesylate for Parkinson’s disease?
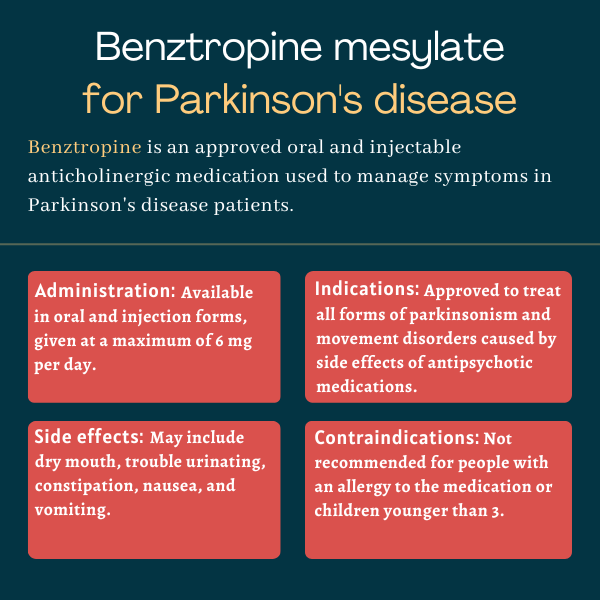
Benztropine mesylate is an approved therapy, available in oral and injection forms, that’s used as an add-on to other medicines to help ease the symptoms of Parkinson’s disease. It also can be used to manage uncontrolled movements that develop as a side effect of certain antipsychotic therapies.
The medication originally was marketed under the brand name Cogentin, by Merck, but that brand name was discontinued due to reasons other than safety or effectiveness issues. Generic formulations of the medication are still available in the U.S.
Therapy snapshot
| Brand name: | Available as a generic medication only |
| Chemical name: | Benztropine mesylate |
| Usage: | Used as an add-on therapy to manage symptoms of Parkinson’s disease and to treat movement problems occurring as a side effect of antipsychotic therapy |
| Administration: | Oral tablets and intravenous or intramuscular injection |
How does benztropine mesylate work?
Parkinson’s disease is caused by the death and dysfunction of cells in the brain that are responsible for producing dopamine, a neurotransmitter, or signaling molecule, that nerve cells use to communicate with each other.
Normally, brain signals using dopamine and another neurotransmitter called acetylcholine help to regulate movement. In Parkinson’s disease, however, these signals become unbalanced, with not enough dopamine for the amount of acetylcholine.
Benztropine is believed to be effective in Parkinson’s mainly by acting as an anticholinergic, or a medication that blocks the activity of acetylcholine. By reducing the strength of acetylcholine signaling, it’s thought that anticholinergic medications like benztropine help to rebalance these brain signals, thereby easing Parkinson’s symptoms.
Who can take benztropine mesylate?
Benztropine was approved by the U.S. Food and Drug Administration in 1954 as a treatment for all forms of parkinsonism, which includes Parkinson’s disease as well as other related disorders that are marked by similar motor symptoms.
The medication also is indicated in the U.S. as a treatment to help manage extrapyramidal reactions, meaning uncontrolled movements, that emerge as side effects of certain treatments for psychosis.
Who should not take benztropine mesylate?
Benztropine is contraindicated, or not recommended, for:
- anyone with an allergy to the therapy or any of its ingredients
- children younger than age 3.
If used in children older than 3, it should be given with caution.
The medication also should generally not be used in patients with certain conditions, including:
- tardive dyskinesia, which is marked by involuntary, repetitive movements as a side effect of certain medications
- angle-closure glaucoma, an eye disease that can lead to a sudden increase in eye pressure and cause eye pain and vision loss.
Patients prone to fast heart rates, known as tachycardia, and those with enlarged prostates, or prostatic hypertrophy, should be closely monitored during treatment with benztropine.
How is benztropine mesylate administered in Parkinson’s?
Benztropine mesylate is available in tablets at dosage strengths of 0.5 mg, 1 mg, and 2 mg for oral administration, which may be given without any specific regard for meals.
The therapy also is available as an injection at a dosage strength of 1 mg per mL, which is typically used only if patients aren’t able to swallow oral versions of the drug. The injection is more commonly given into the muscle; it also may be given directly into the bloodstream, but this is rarely done because it’s more dangerous and doesn’t offer any notable benefits in terms of treatment efficacy.
Regardless of the route of administration, benztropine mesylate should be started at a low dose, typically 0.5 to 1 mg per day, given at bedtime. The dose then may be gradually increased every five or six days in increments of 0.5 mg, with the goal of finding a personalized dose that can help control symptoms without unacceptable side effects.
For most patients, the final dose is 1 to 2 mg per day, though doses ranging from 0.5 to 6 mg per day may be used.
When patients begin taking benztropine, they should avoid suddenly stopping other antiparkinsonian medications. If there is a need to reduce or stop other medicines, it is essential to do so gradually. Benztropine can be used together with levodopa and carbidopa, in which case adjustments to the dosage may be necessary to maintain the best response.
Benztropine mesylate in clinical trials
The original approval of benztropine mesylate took place before the FDA’s modern standards for drug approval, which were implemented in the 1960s and require clinical trial evidence of a drug’s safety and effectiveness.
However, a clinical trial conducted after its approval, in 1980 in Texas, showed that the medication improves symptoms in some Parkinson’s patients.
The trial compared benztropine mesylate against a placebo in 29 people with mild to moderate Parkinson’s who were taking Sinemet, an immediate-release formulation of carbidopa and levodopa. The participants, who ranged in age from 47 to 79, were first given either benztropine or a placebo on top of Sinemet for 10 weeks. Then, after a five-week washout period, which allowed the drug to be fully eliminated from participants’ bodies, those originally given the therapy took the placebo and vice versa, for another 10 weeks.
Among the participants in the trial, 10 reported greater improvements with benztropine than with the placebo, while three reported better outcomes with the placebo. The rest of the patients had similar responses to both benztropine and the placebo. Clinician-rated measures showed similar outcomes.
The results also suggested small but statistically significant improvements in rigidity, finger tapping speed, and activities of daily living for patients given benztropine.
Common side effects of benztropine mesylate
Common side effects of benztropine mesylate include:
- increased heart rate
- dry mouth
- reduced movement of the digestive tract, called paralytic ileus
- painful or difficult urination
- constipation
- nausea and/or vomiting
- confusion, disorientation, and/or memory impairment
- visual hallucinations
- nervousness
- depression
- numbness of fingers
- blurred vision and/or dilated pupils
- skin rash
- heat stroke and/or fever.
Hazardous tasks
Benztropine may cause impairment of physical or mental abilities that can make tasks like driving a car dangerous. Patients should exercise caution until they know how the medication affects them.
Behavioral changes
In susceptible patients, large doses of benztropine may lead to mental confusion, visual hallucinations, and excitement. For those with mental disorders, there is a chance of heightened mental symptoms. It is important to closely monitor patients with mental disorders, particularly at the start of treatment or if the dosage is raised.
Body temperature increase
Benztropine can reduce sweating, which may increase the risk of a patient’s body temperature rising dangerously high, especially for individuals who are regularly physically active or in hot environments. Patients and clinicians should discuss these potential risks, and dosage of the medication may need adjusting so that the body’s ability to regulate its own temperature is not impaired.
Combinations with other drugs
Patients who are taking benztropine in combination with other anticholinergic therapies and/or other medications that alter dopamine activity should tell their healthcare providers at once if they experience any digestive complaints, fever, or heat intolerance, specifically an inability to cool down.
Paralytic ileus or reduced movement of the digestive tract, heat stroke, and hyperthermia, or excessively high body temperature, have occurred in patients given benztropine in combination with phenothiazines, which are a class of antipsychotic medications, and/or tricyclic antidepressants. Some of those cases were fatal, highlighting the need for prompt care if such symptoms are observed.
Use in pregnancy and breastfeeding
Benztropine has not been studied during pregnancy, so it’s unknown if it can cause damage to a developing fetus. Patients who are pregnant or are planning to become pregnant should discuss with their healthcare provider whether it is safe to use benztropine in that situation.
It’s generally recommended that anticholinergic drugs like benztropine should not be used while breastfeeding as they can interfere with milk production.
Parkinson’s News Today is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recent Posts
- Immune T cell response may detect Parkinson’s before symptom onset
- Bezisterim clinical trial uses hybrid design to promote accessibility
- Parkinson’s advocacy groups call for ‘robustly funded, collaborative NIH’
- I may be overprotective, but it’s progress, not perfection
- Living with Parkinson’s reminds me what friends are for
Related articles