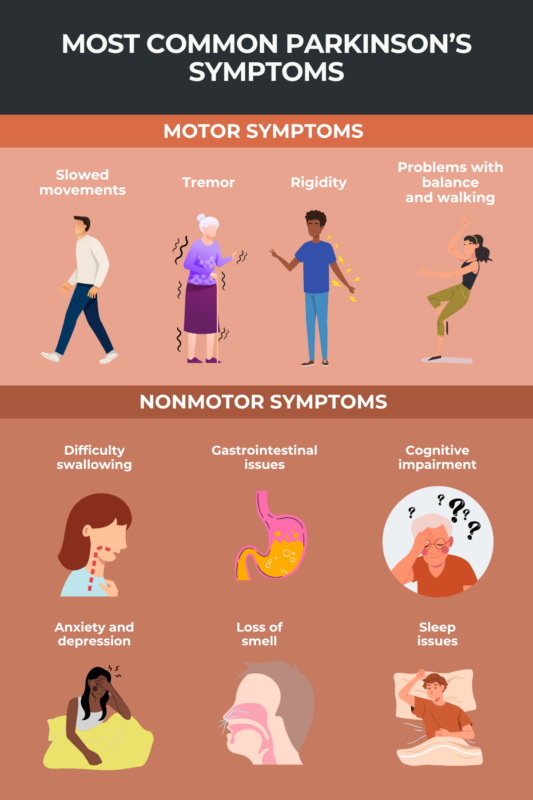
FAQs about Parkinson's disease symptoms
Like many other symptoms of Parkinson’s, tremor is caused by a lack of dopamine signaling. Dopamine is a chemical that nerves use to communicate with each other and the rest of the body. Parkinson’s is caused by the death and dysfunction of brain cells responsible for making dopamine.
Although Parkinson’s disease symptoms tend to worsen over time, how quickly these symptoms progress varies from patient to patient, and it’s currently difficult to make accurate predictions about the speed of disease progression.
While Parkinson’s symptoms tend to get progressively worse over time, symptom severity can vary from day to day and even from hour to hour. Symptoms that cause problems on one day may be less problematic the next. Medications to control symptoms may help to improve the experience of living with Parkinson’s disease, but no treatments are currently available that can slow or stop the overall progression of the disease.
 Fact-checked by
Fact-checked by