Parkinson’s Foundation details essential steps to better hospital care
Group, noting unintended risks, urges 'need to advance overall patient safety'
Written by |
People with Parkinson’s face risks during hospital stays, even when admitted for reasons other than the neurodegenerative disease itself, leading researchers to urge hospitals and health systems to adopt better practices, such as those recommended by the Parkinson’s Foundation.
“Patients with Parkinson’s disease are at increased risk for harm when they are hospitalized. To date, these risks have received little attention and intervention to reduce them — but it does not need to be this way,” Peter Pronovost, MD, PhD, chief quality and transformation officer at University Hospitals Cleveland Medical Center, wrote in an email response to Parkinson’s News Today.
These risks include a worsening of disease motor symptoms such as rigidity and problems with balance, which can lead to falls. Parkinson’s nonmotor symptoms, meanwhile, can affect mental well-being, and patients may feel confused, disorientated, and anxious. If not managed well, these complications can extend hospital stays and lead to a discharge to a care facility, with cumulative medical costs.
More than 300,000 Parkinson’s patients in the U.S. are hospitalized each year, the Parkinson’s Foundation notes. “We understand that these rising numbers and the significant negative impact on health outcomes, underscore the critical need to heighten awareness of this problem, advance overall patient safety and create solutions to improve the lives of people living with [Parkinson’s],” John Lehr, its president and CEO, said in a foundation press release.
Unusual rates of unintended harm mark hospital stays with Parkinson’s disease
“The Parkinson’s Foundation published a set of evidence-based and practical recommendations that can reduce risks to people with [Parkinson’s disease]. We urge health systems to implement these interventions in their journey toward zero harm,” Pronovost said.
A commentary on those recommendations by Pronovost and other scientists in the U.S., “Protecting Parkinson’s Patients: Hospital Care Standards to Avoid Preventable Harm,” was published in The Joint Commission Journal on Quality and Patient Safety.
Hospitals often treat people with Parkinson’s, but staff there may not fully understand their needs, reflecting a lack of disease-specific training and standard protocols. Without clear care guidelines, complications can happen, with a likelihood of longer hospital stays and more frequent readmissions.
“People with Parkinson’s … face disproportionate rates of preventable and unintended harm in the acute care hospital setting, regardless of the reason for admission,” the scientists wrote.
Parkinson’s Foundation recommendations for hospital practices include customizing medication schedules to align with a patient’s home routine, ensuring timely administration of medication, avoiding contraindicated medications — particularly those that block dopamine, like drugs to combat nausea and antipsychotics, or those used for sedation or pain — promoting safe and frequent movement to avoid motor deterioration, and early screening for difficulties swallowing (dysphagia).
Problems noted include a failure to give Parkinson’s medications at set times
“These [recommendations] … can quite literally mean the difference between life and death for someone like me,” said Cindy Finestone, who lives with Parkinson’s. “Even if you think you’ve done all the right things to arrive at the hospital completely prepared, you just don’t realize how bad things can be until it happens to you.”
Finestone added that a recent hospital stay for a routine surgery led to “complications from a near fatal medication interaction.”
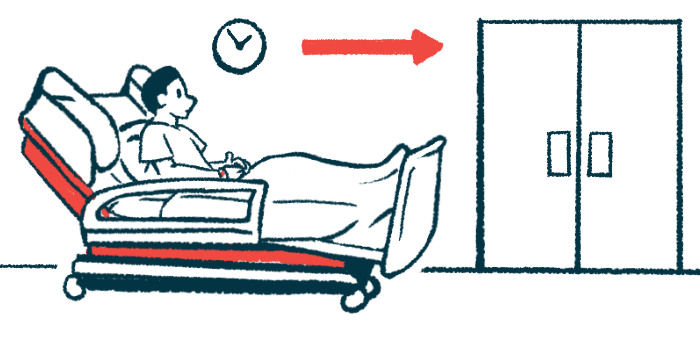
In its report, the foundation noted that 3 out of 4 hospitalized Parkinson’s patient are not given their medicines in a timely manner, recommending that disease treatments always be given within 15 minutes of the person’s at-home regimen. A patient’s hospital stay, it also noted, can be up 14 days longer than that of a peer without Parkinson’s, and it reports that an estimated 63% of hospitalized patients are discharged annually to a specialized facility, while a majority — 51% — will be readmitted to a hospital within a year.
While these recommendations align with broader goals of better and safer hospital care, implementing them requires commitment from both hospitals and health systems, from customizing medication schedules for hospitalized patients rather than relying on default schedules, to requiring annual and disease-specific staff training.
“Despite growing consensus on these [recommendations], hospitals and health systems face knowledge and resource constraints that limit successful implementation. For example, care team awareness of preventable harm among [Parkinson’s] patients is low,” the scientists wrote.



