Distinct immune responses may detect Parkinson’s before symptoms
Stimulation-based tests may help reveal biomarkers for disease progression
Written by |
People in the presymptomatic stages of Parkinson’s disease have distinct patterns of stimulated immune responses relative to those with clinically diagnosed disease or individuals who do not have Parkinson’s, according to a new study.
In particular, the release of certain immune signaling proteins from isolated and stimulated immune cells could distinguish between the prodromal stage (the period between the appearance of initial symptoms and full disease development) and healthy individuals with an accuracy of up to 96%, data show.
“Stimulation-based assays have the potential to reveal novel biomarkers for patient stratification and progression,” researchers wrote.
The study, “Peripheral immune cell response to stimulation stratifies Parkinson’s disease progression from prodromal to clinical stages,” was published in Communications Biology.
Parkinson’s is caused by the progressive death of dopaminergic neurons, or the brain cells that produce dopamine, which is a chemical messenger involved in motor control. The resulting drop in dopamine levels leads to Parkinson’s motor symptoms.
Dopaminergic neurons are lost before Parkinson’s motor symptoms emerge
However, by the time motor symptoms emerge, most dopaminergic neurons have already been lost, which underscores the need for biomarkers that facilitate an early diagnosis.
Early indicators of nerve degeneration can occur many years before the onset of motor symptoms, called the prodromal stage. These include a loss of the sense of smell (hyposmia), constipation, and REM sleep behavior disorder (RBD), where individuals act out their dreams during REM sleep. About 80% of people with this sleep disorder will develop a neurodegenerative disease within 10 years of an RBD diagnosis, and nearly half of these develop Parkinson’s.
“Thus, studying individuals with [RBD] could reveal novel biomarkers for earlier diagnosis of [Parkinson’s] and grant insight into the mechanisms which drive disease progression prior to the onset of classical [Parkinson’s]-associated motor symptoms,” the researchers wrote.
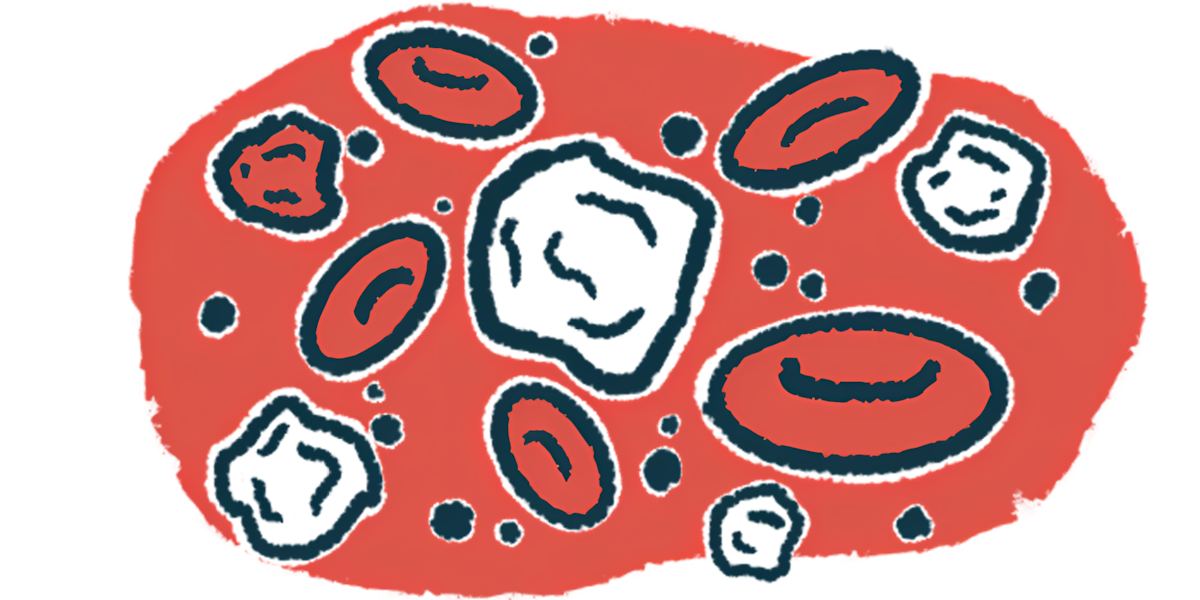
Immune system dysregulation has long been implicated in the development of Parkinson’s. For example, altered levels of immune signaling proteins (cytokines) and certain immune cells have been detected in the bloodstream of Parkinson’s patients. Still, diet, circadian rhythms, and environmental exposures can influence many of these changes, limiting their effectiveness as biomarkers.
Therefore, University of Florida researchers investigated whether the immune response to stimulation is altered in prodromal patients relative to those in different stages of Parkinson’s.
To test this hypothesis, the team isolated immune cells from the blood of 15 individuals with prodromal signs, 27 with early-stage Parkinson’s (within two years of diagnosis), and 30 with moderate-stage Parkinson’s (within two to 10 years of diagnosis). A group of 21 age- and sex-matched healthy individuals served as controls. The prodromal group had RBD, with most showing some related symptoms, such as constipation and hyposmia.
From the immune cell mix, two types of white blood cells called monocytes and T-cells were isolated and stimulated, and the immune response was assessed by measuring the levels of released cytokines.
Stimulation test shows different cytokine release depending on disease stage
Results showed monocyte stimulation boosted the release of several pro-inflammatory cytokines in the prodromal stage but not in the early and moderate stages of Parkinson’s. Similarly, cytokine release was higher in stimulated T-cells from prodromal patients than those with moderate-stage Parkinson’s.
Monocyte secretion of two cytokines, TNF and interleukin-1-beta (IL-1-beta), was able to distinguish prodromal patients from healthy controls with an accuracy of 96% and 82%, respectively. Prodromal Parkinson’s could also be distinguished from healthy controls with T-cell secretion of IL-1-beta, with an accuracy of 79%, and IL-8, with an accuracy of 71%.
TNF secretion from T-cells alone could differentiate early-stage disease from healthy controls with an accuracy of 79%. In addition, T-cell secretion of TNF, IL-2, and IL-10 distinguished moderate-stage from controls, with accuracies ranging between 70% and 77%.
“These results suggest that cell-type specific cytokine secretion … could be a useful component for biomarker-based predictive models aimed at distinguishing healthy individuals from those with [Parkinson’s], including at the prodromal stage,” the team wrote.
To understand the mechanisms underlying altered immune responses in Parkinson’s, researchers examined the health of mitochondria, the cell’s energy source, which can affect the release of cytokines. Mitochondrial dysfunction is known to trigger inflammation and impair immune cell function, both of which may contribute to altered immune responses in Parkinson’s.
Stimulation revealed deficits in the health of mitochondria in CD8-positive T-cells, also called cytotoxic T-cells, in moderate-stage Parkinson’s. Moreover, healthier mitochondria in these cells were associated with higher release of IL-1-beta, IL-8, and IL-10 in prodromal individuals.
“Dysregulated mitochondrial health in immune cells may contribute to peripheral inflammation and [Parkinson’s] progression,” the team noted.
“This work demonstrates that peripheral blood immune cells from prodromal [Parkinson’s] patients display a distinct pattern of stimulation-dependent immune dysregulation relative to [healthy controls] and clinically diagnosed [Parkinson’s] groups,” the researchers wrote.