Activating Specific Neurons in Brain Restores Movement in Mouse Model
Activating a particular subpopulation of nerve cells in a specific region of the brain — caudal glutamatergic neurons in the pedunculopontine nucleus — can normalize movements in mouse models of Parkinson’s disease, a study reports.
Its results suggest that finding ways to specifically stimulate these neurons could ease motor symptoms in Parkinson’s patients.
The study, “Targeted activation of midbrain neurons restores locomotor function in mouse models of parkinsonism,” was published in Nature Communications.
Parkinson’s is caused by the death and dysfunction of nerve cells in the brain that make the signaling molecule dopamine. The lack of this signaling molecule causes motor symptoms like bradykinesia (slow movements) and akinesia (lack of movement).
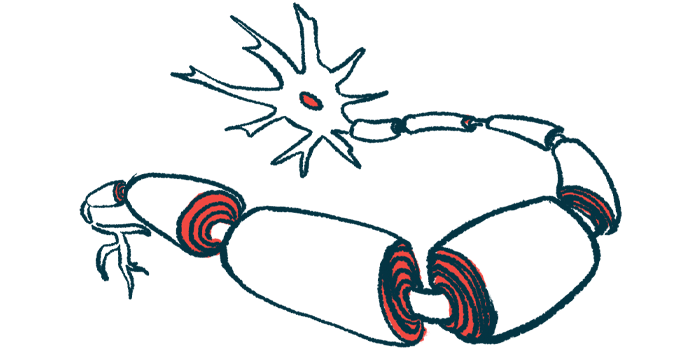
During movement, dopamine signals are normally released from a brain region called the basal ganglia, and go on to activate another brain region called the pedunculopontine nucleus (PPN). The PPN, part of the brainstem, then sends further signals out to help spur body movement.
Based on this known flow of signaling, it has been suggested that activating the PPN could help to normalize its activity, lessening motor symptoms. Deep brain stimulation, or DBS, is a surgical technique that involves implanting a device in the brain to electrically stimulate certain regions.
Using DBS to stimulate the PPN in Parkinson’s patients has been tried, but results have been inconsistent. It is most effective, the researchers noted, in easing tremor but not problems with walking or frozen gait.
“Initial results from clinical trials with DBS of the PPN had very variable effect on movement recovery, particularly in patients who experience freezing of walking,” Ole Kiehn, PhD, a professor of neuroscience at the University of Copenhagen and study co-author, said in a press release.
Working alongside Debora Masini, PhD, Kiehn conducted a series of tests to see whether better results might be possible if only certain cells in the PPN were targeted.
Basically, the PPN contains three types of neurons, called glutamatergic, cholinergic, and GABAergic. These neurons are defined by the particular chemicals they release when activated, which in turn affects their activity — for example, glutamatergic release a signaling molecule (glutamate) that usually activates other neurons, while the molecule made by GABAergic cells tends to stop other neurons from activating.
Established evidence suggests that cholinergic neurons in the PPN play a comparatively small role in dictating movement, so here the scientists focused specifically on the glutamatergic and GABAergic neurons.
The pair created a series of mouse models where, using lights or chemicals, they could specifically activate a particular group of neurons. Of note, the researchers focused on caudal (towards-the-tail) PPN neurons, which are more important for controlling movement than their counterparts nearer the front of the head.
They then tested the effects of activating the neurons in two Parkinson’s models generated by treating mice with chemicals that block dopamine signaling. Mice in these models exhibit many motor abnormalities similar to what is seen in patients.
“We systematically compared stimulation of different locations and cell types in a series of complementary experiments,” Masini said.
Results broadly showed that increasing the activity of glutamatergic neurons in the PPN led to a normalization of movements. By comparison, activating GABAergic neurons did not normalize movements, and neither did activating glutamatergic neurons in a nearby brain region called the cuneiform nucleus.
“When we stimulated these specific neurons in the caudal area of the PPN, the animals were able to walk normally, across longer distances and with normal walking speed, as opposed to before the stimulation, where they would display symptoms” of Parkinson’s, Masini said.
She added that the result “strongly indicates these excitatory neurons in the caudal PPN are an ideal target for recovery of movement loss.”
The findings also may explain why stimulating the entire PPN region failed to yield consistent benefits, as such broad stimulation would be expected to activate both glutamatergic and GABAergic cells.
“Since cell-specific stimulation of caudal GABAergic PPN neurons does not revert locomotion to a normal locomotor phenotype in our parkinsonian model it suggests that concomitant stimulation of glutamatergic and GABAergic neurons in a DBS setup may contribute to the unreliable results in clinic studies,” the researchers wrote.
Directly translating these results into people, they noted, would require an ability to control the activity of individual cell types, for example, by genetically engineering the cells so that they activate in response to a chemical. While this is not currently feasible, it “might be possible in a not too far future,” the researchers wrote.
In the meantime, they suggest that DBS for Parkinson’s patients should try to target glutamatergic neurons in the PPN as much as possible.