Researchers Design New Approach to Help Medications Enter the Brain

Researchers have developed a new method of temporarily opening the selective blood-brain barrier (BBB) to allow therapeutic molecules greater access to the brain.
Difficulties in developing molecules that can cross this barrier have long hindered the development of treatments for neurological diseases, like Parkinson’s disease. The technique could now help advance better treatment for these conditions, the researchers noted.
The approach — which combines tiny gas bubbles and ultrasound — is being tested in patients with brain cancer and Alzheimer’s disease, and has so far shown no side effects, according to a press release.
“This is a big step towards better treatment for various brain diseases,” said Catharina de Lange Davies, PhD, a professor in the department of physics at the Norwegian University of Science and Technology, and a study author.
“We think these results are exciting and encouraging,” she added.
The study, “Acoustic Cluster Therapy (ACT®) enhances accumulation of polymeric micelles in the murine brain,” was published in the Journal of Controlled Release.
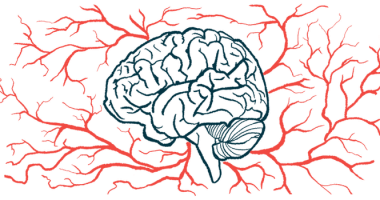
What is the blood-brain barrier?
A highly selective network of tightly knit cells, the BBB serves to prevent potentially harmful substances, like toxins or pathogens, that may be circulating in the body from entering the brain.
The barrier is not impenetrable — it lets substances like water, certain gases (e.g. oxygen), and some fat-soluble small molecules through — but virtually all large molecules and most small ones are prevented from crossing over.
While it effectively protects one of the body’s most vulnerable organs, this also means that many medications have difficulty entering the brain, posing a significant challenge to developing therapeutics for neurological disorders like Parkinson’s.
Researchers previously developed a technique to help overcome this obstacle, which involves the use of tiny gaseous “microbubbles” and focused ultrasound at the BBB. The microbubbles are injected into the bloodstream, then an ultrasound is applied. The energy from the ultrasound causes the microbubbles to vibrate and push against the blood vessel walls that comprise the BBB.
This mechanical pressure creates openings in the BBB that facilitate the entry of therapeutic molecules.
Davies and her team collaborated with EXACT Therapeutics to develop a new type of bubble — larger than those previously used — that could help to create bigger gaps. They dubbed the approach acoustic cluster therapy (ACT).
In ACT, a small negatively charged microbubble is attached to a positively charged drop of oil and injected into the bloodstream. When a high-frequency ultrasound is directed at the brain, the bubble vibrates and transfers its energy to the oil droplet. The two then merge into a single, enlarged bubble with 1,000 times more volume than other commercially available bubbles.
Due to its size, the microbubble comes into greater contact with blood vessel walls at the BBB. A second, lower frequency ultrasound causes the larger bubbles to vibrate and open the BBB, as with other approaches.
In the study, the team tested how well the microbubbles worked in mice. Some mice received ACT and others received a sham injection without microbubbles. MRI imaging showed that ACT-treated mice had more enhanced opening of the BBB which lasted at least 24 hours, but was largely reversed after 48 hours.
When a special fluorescent dye was administered to the mice, the researchers saw that more of it was able to enter the brain with ACT. Similarly, when mice were injected with nanoparticles — tiny carriers often used to deliver therapeutic materials — more were able to enter the brain after the microbubble treatment.
No evidence of blood vessel bleeding, tissue damage, or inflammation were observed after ACT.
“The method increases the permeability of the blood-brain barrier. It also increases the uptake of large molecules and nanoparticles in the brain,” de Lange Davies said. “In our mouse experiments, we’ve shown that the blood-brain barrier closes after about one day, and we haven’t found any significant damage to the brain tissue.”
The researchers wrote that the findings take “a principal step in enabling improved treatment of various brain diseases,” noting that ACT may be particularly effective when used in combination with nanoparticle carriers.