Better Biomarkers Needed to Diagnose, Predict Risk of Mild Cognitive Impairment
There still are no reliable biomarkers for early detection, or to characterize and predict risk of dementia, in Parkinson’s disease, according to a recent analysis.
Several studies on the cognitive deficits, progression to dementia, potential biomarkers and the mechanisms underlying Parkinson’s disease mild cognitive impairment (PD-MCI) were analyzed by University College London researchers in the review study “Mild Cognitive Impairment in Parkinson’s Disease—What Is It?,” which was published in the journal Current Neurology and Neuroscience Reports.
Large-scale studies have shown that PD-MCI is not only important, but also common, even at the earliest stages of Parkinson’s disease. In fact, MCI signs can be detected before the onset of Parkinson’s motor symptoms.
About half of Parkinson’s patients with cognitive impairment will progress to dementia in the first 10 years after diagnosis. But considerable variation exists among this patient population regarding the type of cognitive domains affected, the timing, severity and risk of progression to dementia.
Accordingly, PD-MCI is emerging as an intermediate stage between normal cognition and dementia, similarly to the stage of amnestic mild cognitive impairment in Alzheimer’s disease.
Epidemiological studies report that 25 to 50 percent of Parkinson’s patients have MCI, depending on the population and the clinical setting. Identifying individuals with early signs of PD-MCI or at risk of dementia is important to provide early interventions, estimate prognosis, and discover therapeutic targets.
In an effort to clarify the diagnosis of PD-MCI, a task force from the International Parkinson and Movement Disorder Society (MDS) provided a unified definition. According to the new criteria, PD-MCI is defined as an “insidious decline in cognitive abilities reported by patient or informant or observed by the clinician, not caused by other comorbidities.”
Unlike dementia, MCI deficits are detectable, but do not interfere with patients’ autonomy.
The nature and severity of PD-MCI is quite variable. The dominant manifestation does not involve memory. But there are other subtypes with deficits in attention, memory, executive function, psychomotor speed and visuospatial abilities. In some people the deficits can involve multiple cognitive domains.
The MDS has recommended a battery of tests to assess involvement of single or multiple domains and report exactly which domains are affected.
In general, patients with PD-MCI are at higher risk of progressing to dementia than Parkinson patients without MCI. Importantly, studies report that 11 to 28 percent of patients with PD-MCI revert to normal cognition during follow-up.
The variability of these results is likely to reflect differences in study populations, assessment methods and definitions.
Some factors can increase risk of cognitive deficits in Parkinson’s, including being older than 70, akinetic rigid phenotype (freezing and/or falls), poor verbal fluency and higher rates of comorbidities. Higher rates of progression to dementia are associated with older age, depression and a non-tremor clinical manifestations.
Exploring biomarkers
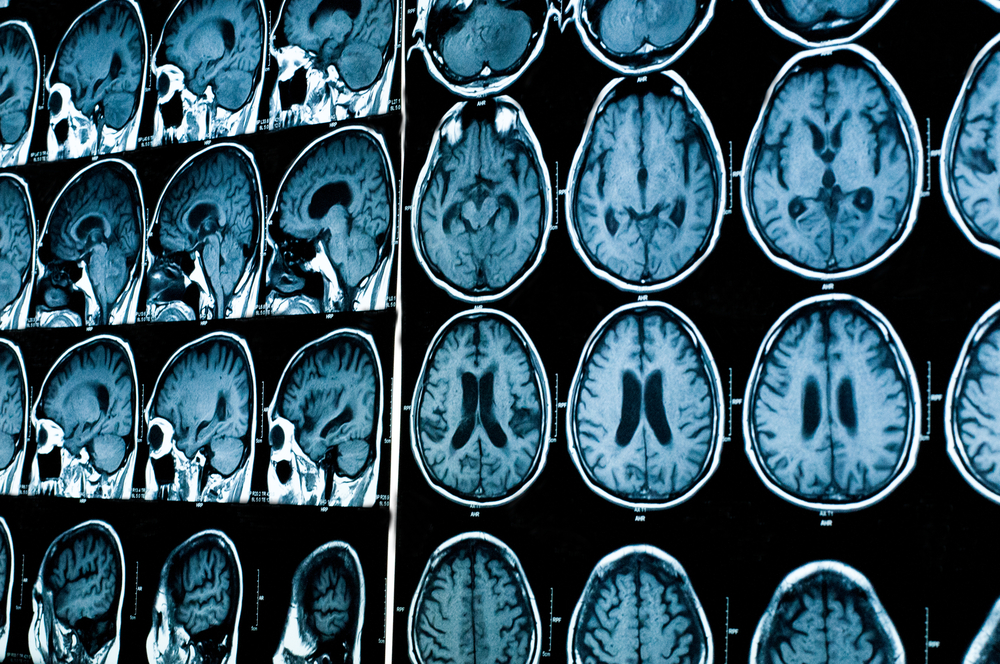
Biomarkers such as amyloid beta protein in the cerebrospinal fluid, and magnetic resonance imaging of the brain, may become important for providing insights into mechanisms of cognitive involvement and for accessing disease progression.
The mechanisms underlying PD-MCI likely involve a combination of factors. Brain aggregates of the proteins alpha synuclein, beta amyloid and tau — the latter two also characteristic of Alzheimer’s disease — are likely to play a role.
Besides, some studies suggest that changes in specific neurotransmitters — chemical messengers used to communicate between neurons, including acetylcholine, noradrenaline and dopamine — also contribute to cognitive impairment.
Some questions regarding PD-MCI remain unresolved. One of them is the distinction between dementia with Lewy bodies (intracellular accumulations of alpha synuclein) and Parkinson’s dementia.
Dementia with Lewy bodies emerges early, before or within the first year of Parkinsonism, while Parkinson’s dementia is defined as a progressive decline appearing at least one year after motor symptoms are noticeable.
However, given the reports of people with cognitive deficits even before characteristic manifestations of Parkinson’s, perhaps cognitive impairments are the first signs of Parkinson’s disease and may start earlier than believed.
Some studies report that some PD-MCI sub-groups, particularly those with deficits in visuospatial performance, are at the highest risk of dementia.
This underscores the need for better assessment methods and biomarkers of PD-MCI to allow well-defined characterizations of the cognitive deficits and predict who is more prone to dementia.
Although the antipsychotics Nuplazid (pimavanserin) and Clozaril (clozapine) are the only therapies shown to improve Parkinson’s disease psychosis (PDP) symptoms without impairing motor function, there currently are no pharmacological treatments specifically for PD-MCI.
The effect of current experimental therapies on cognition is unknown. Some studies suggest that cognitive training can improve overall cognition in Parkinson’s patients, although the effect seems small.
Physical exercise shows more promising results. Several studies report that moderate intensity aerobic exercises performed two to three times a week lead to some improvement in executive and language functions.
However, Acadia Pharmaceuticals, Nuplazid’s manufacturer, is planning to conduct additional studies of the therapy in PD psychosis patients with a broader range of cognitive abilities and formal cognitive diagnoses, including mild cognitive impairment and dementia.
“Maintaining wide definitions, with poorly differentiated cognitive profiles, prevents accurate comparisons across studies,” researchers wrote. “There is clearly a need for better cognitive phenotyping to enable well-defined sub-groups that are more likely to show similar rates of disease progression.”
“Recognizing the earliest stages of cognitive involvement will allow disease stratification and personalized treatment, with the potential for early intervention. It will enable better-powered clinical trials, and potential outcome measures, ultimately to develop treatments to prevent the progression of dementia in PD,” the review concluded.






