Alpha-synuclein prods neurons’ protein gain, causing them to die
In study, researchers explored how disrupted proteostasis leads to Parkinson’s
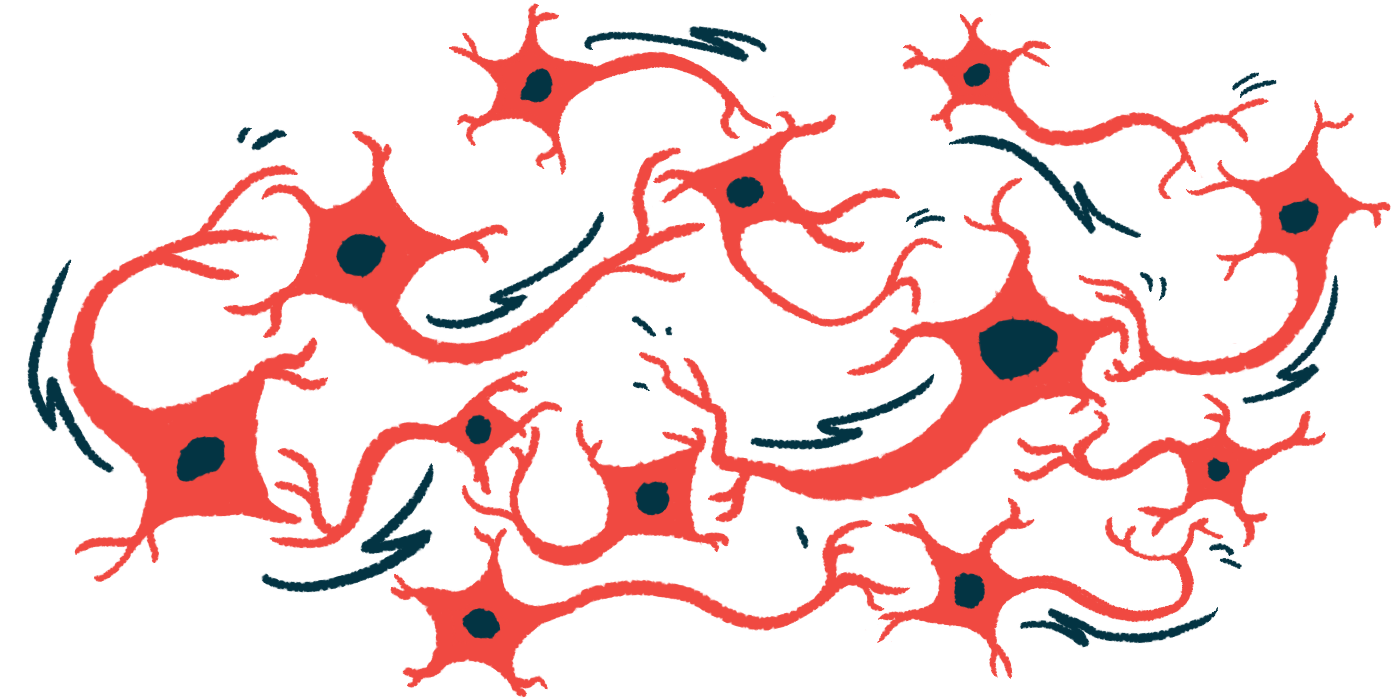
Alpha-synuclein, the protein that builds up into toxic clumps in Parkinson’s disease, may trigger neurons (nerve cells) to increase their production of new proteins, ultimately causing them to die, according to a recent study.
“Parkinson’s disease has major impacts on quality of life for patients, but also for their caretakers and loved ones,” Ted M. Dawson, MD, PhD, who led the study and is a professor of neurology at the Johns Hopkins University School of Medicine, said in a press release. “We hope that research like this will provide mechanistic, molecular-based therapies that can actually slow or halt the progression of Parkinson’s disease.”
Dawson directs Johns Hopkins University’s Institute for Cell Engineering.
The study, “Enhanced mTORC1 signaling and protein synthesis in pathologic alpha-synuclein cellular and animal models of Parkinson’s disease,” was published in Science Translational Medicine.
Alpha-synuclein and disrupted protein regulation
Proteostasis refers to the balanced regulation of proteins in the body. When this balance is disrupted, it can contribute to developing Parkinson’s, a disease best known for motor symptoms that result from the loss of dopamine, a neurotransmitter essential for movement.
While it’s not known what causes or triggers the death of dopamine-making cells in Parkinson’s, the abnormal clumping of alpha-synuclein in brain cells may be one factor.
To understand how disrupted proteostasis contributes to Parkinson’s, Dawson and his colleagues used lab-grown neurons, flies, and mice to see which proteins interact with misfolded alpha-synuclein in neurons.
They found that misfolded alpha-synuclein interacted with tuberous sclerosis protein 2 (TSC2), which normally prevents cells from growing too large and dividing uncontrollably.
When misfolded alpha-synuclein interacted with TSC2, it prevented the protein from interacting with TSC1, another protein that keeps the mammalian target of rapamycin (mTOR) in check.
Signals transmitted via mTOR are important for the brain’s growth and development. In the absence of TSC1, mTOR bound to other proteins to form mTOR complex 1 (mTORC1), which increased the production of new proteins, leading to neurodegeneration.
In fly and mouse models of Parkinson’s, treatment with rapamycin — an immunosuppressant that works by inhibiting mTOR— both prevented excessive protein production and the death of dopamine-producing neurons, but also eased motor symptoms. Rapamycin is often used to prevent transplanted organs from being rejected and is being explored for treating certain cancers and promoting healthy aging.
The disruption of the TSC1-TSC2 interaction was confirmed in samples of post-mortem brain tissue of people with Parkinson’s, suggesting these proteins may provide targets for treating the disease.
In the future, scientists might, for instance, create medications with properties similar to rapamycin, but that are designed to act on the brain and preserve neurons that produce dopamine. This approach could spare patients from a number of side effects. Alternatively, targeting TSC2 might aid in achieving a similar effect.
More research is needed to validate these potential targets. How excessive protein production leads dopamine-producing neurons to die also remains unclear. “The molecular mechanism of this deregulation is poorly understood,” the researchers wrote.