New Method Devised to Generate Dopaminergic Neurons
Using skin cells of Parkinson's patients may further understanding of the disease
Researchers have devised a new method to generate dopamine-producing neurons from skin cells of Parkinson’s disease patients, a process that could be used to better study the molecular mechanisms of the disease and develop new treatments.
The cells retained many relevant aspects of the disease, including the accumulation of alpha synuclein, and captured age-related changes that most animal and cellular models fail to recapitulate.
“Of importance here is that the aging signature of the donor cell is maintained during direct conversion, … which uniquely allows for modeling age-related aspects of” Parkinson’s disease, researchers wrote.
The study, “Age-related pathological impairments in directly reprogrammed dopaminergic neurons derived from patients with idiopathic Parkinson’s disease,” was published in the journal Stem Cell Reports.
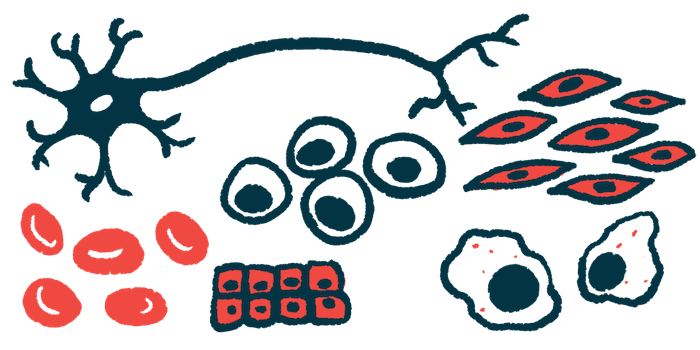
Parkinson’s disease is characterized by the progressive loss of dopaminergic neurons — neurons that communicate by releasing a major chemical messenger in the brain called dopamine.
While a hallmark of disease is the accumulation of toxic alpha-synuclein clumps inside nerve cells, the exact mechanisms leading to disease onset and development remain poorly understood. That is mostly because there is a lack of appropriate models that accurately mimic disease processes.
Induced pluripotent stem cells, or iPSCs, often are used to study genetic contributions to disease. iPSCs are produced by collecting mature cells — usually cells isolated from skin samples — and reprogramming them into stem cells, which have the capacity to differentiate into virtually any other cell type in the body under the right conditions.
When generated from an individual patient, the stem cells will carry the same disease-causing mutations the patient does. Using specific chemicals, the stem cells can mature into nerve cells or other cell types of interest, and then be studied in the lab.
Age is important
However, as in most other models of Parkinson’s, one particular feature that is not captured in these cells is age, which is “the biggest risk factor for developing this condition,” the researchers wrote. They also fail to retain the epigenetic features of the patient, which are chemical modifications to the DNA that determine which genes are read and how active they are.
Now, a team led by researchers in Sweden devised a way to generate dopaminergic neurons from skin cells directly, without going through the stem cell intermediate.
The nerve cells were obtained by treating skin cells with an optimal combination of factors required for the normal development and function of dopaminergic neurons. Analyses of the resulting cells showed they were behaving like neurons — they could spontaneously fire electrical signals — and had increased activity of genes related to dopamine, therefore determining the validity of the model.
Using the new method, the researchers generated dopaminergic neurons from 18 Parkinson’s patients, and 10 age- and sex-matched healthy controls. Compared with healthy controls, neurons from Parkinson’s patients had impaired stress-induced autophagy, a natural recycling process in which cells degrade unnecessary or damaged components.
These defects were not observed in the skin cells before they were converted into neurons, confirming that disease features are observed only in neurons.
Notably, neurons obtained from both healthy and Parkinson’s disease patients exhibited characteristics related to the age of the patient. In particular, cells from older patients had a greater accumulation of lysosomes — cell structures responsible for the degradation of molecules inside cells — in their nerve cells.
MAPT gene’s effects
This effect was more pronounced in neurons carrying a form of the MAPT gene associated with faster disease progression and cognitive decline. This gene provides instructions to make the Tau protein, which provides structural stability to neurons.
The patient-derived cells also exhibited other features of cellular aging, such as more cell damage, an age-related gene signature consistent with the age of the donor, and the accumulation of alpha synuclein. In contrast, these age-related features were not observed in iPSCs-derived dopaminergic neurons.
“This effect of age and genetic variance on disease pathology has not been recapitulated in cellular models before, and suggests that direct conversion to [dopaminergic neurons] could be used for differential diagnostics, drug screening, and disease modeling of late-onset neurodegenerative diseases,” the researchers wrote.
Moreover, in neurons derived from skin cells, they detected alpha-synuclein pathology, but not in the neurons derived from iPSC. “The maintenance of age in [skin cell-derived neurons] is important for modeling the [alpha-synuclein] pathophysiology of idiopathic [Parkinson’s disease],” they concluded.
“Future studies using this cellular model will thus contribute to a deeper understanding of the age-associated pathology of [Parkinson’s disease] along with the cellular basis of disease subtypes and variable progression and, by so doing, allow us to better develop and assess novel therapeutic interventions,” they added.







