Mouse Study Implicates Calcium Channel in Neuronal Death in Parkinson’s Disease
A calcium channel called Cav2.3 plays a role in neuronal death, and may be a useful therapeutic target in Parkinson’s disease, suggests a new study done primarily in mice.
The study, titled “Cav2.3 channels contribute to dopaminergic neuron loss in a model of Parkinson’s disease,” was published in Nature Communications.
Motor symptoms in Parkinson’s disease are caused primarily by the death of dopamine-producing (dopaminergic) neurons in a part of the brain called the substantia nigra (SN). It has been well-established that calcium signaling — that is, calcium ions moving in or out (but usually in) of a cell, which is mediated by specialized “channel” proteins — plays an important role in the functioning and survival of these neurons, but the precise mechanisms are still not fully understood.
In the new study, researchers began by measuring the levels of several different calcium channels in these neurons in the brains of mice. They were surprised to find higher levels of Cav2.3 than any other calcium channel; Cav2.3 has never been linked to neurodegeneration (neuron cell death) before.
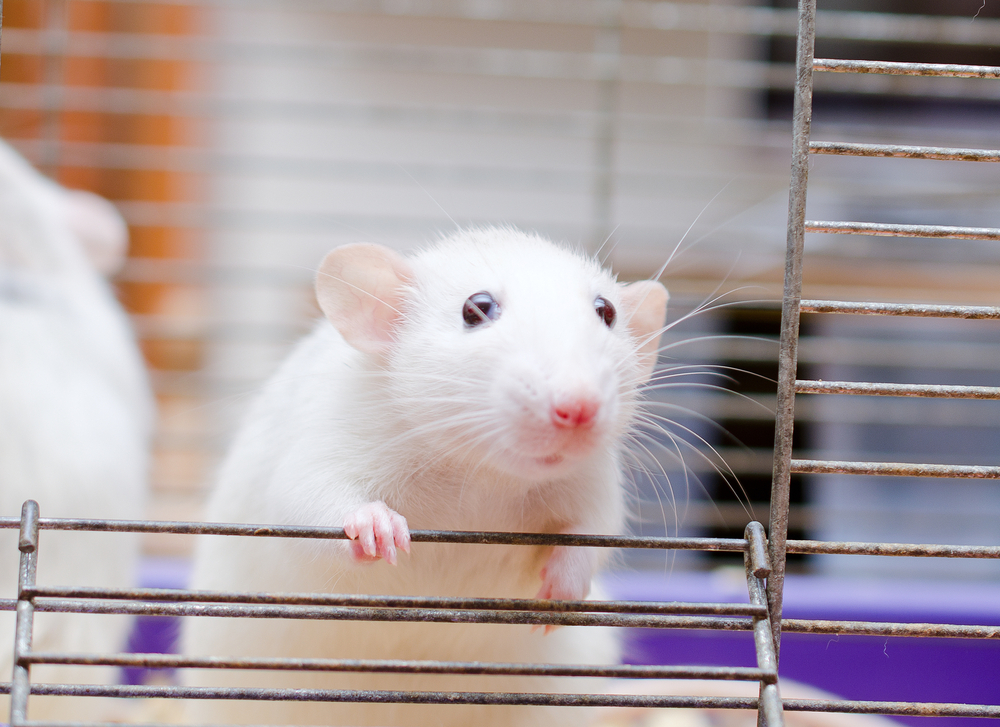
The researchers then used mice that had been genetically engineered so they could not make Cav2.3 and treated them with MPTP (1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine), a chemical that is toxic to neurons and is “the standard model for preclinical testing of neuroprotective Parkinson’s disease therapies in animals,” the researchers wrote.
In wild-type (i.e. with functional Cav2.3) mice, MPTP treatment resulted in the death of about 40% of the dopaminergic neurons in the substantia nigra.
“In stark contrast, we observed no loss of SN dopaminergic neurons in Cav2.3 knockout animals after MPTP treatment,” the researchers wrote. “Taken together, these data identify Cav2.3 as mediator of SN dopaminergic neuron vulnerability to a degenerative stressor.”
The researchers then measured levels of other calcium-related proteins in neurons lacking Cav2.3, in order to identify possible mechanisms for this phenomenon. They found that these cells had increased levels (by about 40%) of a calcium-sensing protein called NCS-1, and they hypothesized that higher levels of this protein might lend the neurons protection from MPTP.
To test this, the researchers treated mice that lacked NCS-1 with MPTP, which resulted in the death of about 60% of the dopaminergic neurons in the SN — significantly more than was seen in wild-type mice.
“NCS-1 thus emerges as protective factor during SN dopaminergic degeneration, of likely relevance to Parkinson’s disease,” the researchers wrote.
Finally, the researchers turned to human cells. They took skin cells from volunteers, and engineered these into a type of stem cell called induced pluripotent stem cells (iPSCs), which were subsequently induced to differentiate into neurons.
The researchers compared iPSC-derived neurons from people without Parkinson’s disease to those of a Parkinson’s disease patient who had a mutation in the GBA gene (such mutations are associated with a high risk of Parkinson’s disease).
No significant differences were found in the amount of Cav2.3 protein; however, levels of NCS-1 were about 40% lower in the neurons from the person with Parkinson’s. Although this does not provide definitive proof, it suggests that similar molecular mechanisms might be at play in human Parkinson’s disease.
“Collectively, our data strongly suggest opposing roles for Cav2.3 and NCS-1 in Parkinson’s disease,” the researchers said, adding that “Cav2.3 is neurodegenerative whereas NCS-1 is protective for SN dopaminergic neurons. Whether this involves any direct functional or molecular interactions between the two proteins must be clarified in future experiments.”
“Cav2.3 and NCS-1 thus emerge as potential targets for neuroprotective therapy,” they added.
Although a recent Phase 3 clinical trial (NCT02168842) using DynaCirc (isradipine) — a medicine used to treat high blood pressure — to block another type of calcium channel, called Cav1.3, showed that it did not protect against Parkinson’s disease, the authors believe that the therapeutic dose given may not have been sufficient to fully inihibit this channel in dopaminergic neurons. Alternatively, inhibiting this specific type of calcium channel may “be protective only under distinct conditions, e.g. before motor symptoms manifest, or in response to transiently elevated dopamine levels during dopamine replacement therapy,” they added.
Currently, the only available Cav2.3 inhibitor (SNX-482) is not suitable to be used in a clinical setting “due to off target effects.” As such, the “development of high affinity, brain-permeable, and selective Cav2.3 channel blockers is warranted,” the researchers said.