Eye neurodegeneration mouse model may aid Parkinson’s research
Mice are lacking the protein VPS35 in their retinal rod cells
Written by |

Researchers have developed a new mouse model that affects nerve cells in the eye that could help in studying disease mechanisms and treatment approaches in Parkinson’s disease.
The mice are lacking the protein VPS35 in specific cells of the eye and developed protein deposits that contain alpha-synuclein, neurodegeneration, and visual defects similar to what’s observed in Parkinson’s patients.
“This is a really unique model involving a pathology that seems more like human Parkinson’s than what we see in other mouse models,” Ching-Hwa Sung, PhD, a professor at Weill Cornell Medicine in New York and the study’s senior author, said in a university press release. “This is the beginning of what we expect to be a very interesting exploration.”
The study, “Mutant mice with rod-specific VPS35 deletion exhibit retinal α-synuclein pathology-associated degeneration,” was published in Nature Communications.
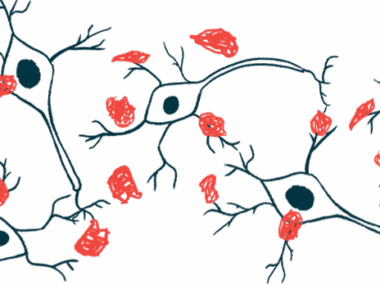
A hallmark of Parkinson’s disease is the formation of Lewy bodies, abnormal and insoluble protein deposits that build up in nerve cells and cause them to degenerate. These Lewy bodies are made up mainly of aggregates of an abnormal and misfolded version of alpha-synuclein.
One place this pathology can be observed is in the eye. More than 80% of Parkinson’s patients develop early vision changes related to the death of nerve cells in the retina, that is, the back part of the eye where light is sensed and converted into electrical signals that are sent to the brain. Lewy bodies have been observed in the retinas of Parkinson’s patients.
A number of proteins are important for clearing away misfolded or otherwise unnecessary proteins and dysfunction in these systems can lead to Parkinson’s.
One protein, VPS35, helps distribute various molecules to where they’re needed, including sending abnormal proteins off for degradation. A mutation in the gene that encodes VPS35’s production has been linked to Parkinson’s disease.
Engineering mice without VPS35 protein
Here, researchers examined the effects of genetically engineering mice to deplete them of VPS35, specifically in rod cells, a main class of light-sensing nerve cells, or photoreceptors, in the retina.
They found that from an early age, rods in the mutated mice lost their physical connections to other nerve cells, called synapses, which led to visual impairments not unlike those observed in Parkinson’s patients. Relative to healthy mice, toxic forms of alpha-synuclein were significantly increased in all layers of the retina of the mutant mice, along with evidence of other structural and functional changes in the retina.
Eventually, the diseased rods started to die off and neurodegeneration was evident. By that time, large protein clumps similar to Lewy bodies could be observed in the eye.
Throughout a series of experiments, the researchers identified a protein network that VPS35 interacts with to exert its effects, including physical interactions with the protein HSC70 that’s important for escorting misfolded proteins to cell compartments to be degraded. A lack of VPS35 caused this normal function of HSC70 to be disrupted, leading to alpha-synuclein aggregation.
The findings indicated VPS35 is important for getting rid of alpha-synuclein clumps and for preventing them from forming in the first place, according to the scientists.
Microglia, the brain-resident immune cells that help engulf and remove waste products like alpha-synuclein became abnormally activated and moved into the retinal region.
Because the cellular processes that occurred when VPS35 was removed from these retinal cells were so similar to what’s seen in Parkinson’s, the scientists think the mice could be used as a model for studying disease mechanisms and developing new treatments.
Advantages of this model include how quickly the disease developed, as well as the fact that other models require direct manipulations to increase toxic alpha-synuclein, whereas that pathology developed on its own in these mice.
“We further propose that the … mouse line is a valuable tool for testing strategies for ameliorating the [alpha-synuclein] lesion and its associated neuronal functional decline,” the researchers wrote.
A surrogate indicator of alpha-synuclein aggregation in the eye was measured with a fundoscope, an ophthalmological device that can visualize the retina. The researchers believe this could be a noninvasive strategy for detecting Parkinson’s disease, which “remains a pressing need.” The researchers are now working with physicians to design a clinical trial that would test this approach.
VPS35 mutations also have been linked to Alzheimer’s disease, so the scientists are planning studies that would use the new mouse model to investigate that neurodegenerative condition.