Mitochondrial DNA damage evident before Parkinson’s: Study
Finding suggests damage may be early cause, not consequence, of the disease
People with REM sleep behavior disorder, a condition that often precedes Parkinson’s disease, frequently have mitochondrial DNA (mtDNA) damage, a study found.
“Patients with REM sleep behavior disorder, both those who subsequently developed Parkinson’s disease and those who did not, had more mitochondrial DNA circulating in the cerebrospinal fluid with deletions — that is, with losses of some fragment of genetic material — than the control group,” Margalida Puigròs, the study’s first author at the University of Barcelona in Spain, said in a university press release.
The “most relevant finding” was “that the amount of DNA with deletions is related to the time it takes for patients with sleep behavior disorder to manifest clinical symptoms of Parkinson’s disease,” Puigròs said.
That implies mtDNA damage is an early cause, not a downstream consequence, of Parkinson’s, which is linked to defective mitochondria and altered levels of cell-free mtDNA in bodily fluids.
The study, “Mitochondrial DNA deletions in the cerebrospinal fluid of patients with idiopathic REM sleep behavior disorder,” was published in eBioMedicine.
Mitochondrial DNA damage may contribute to neurodegeneration
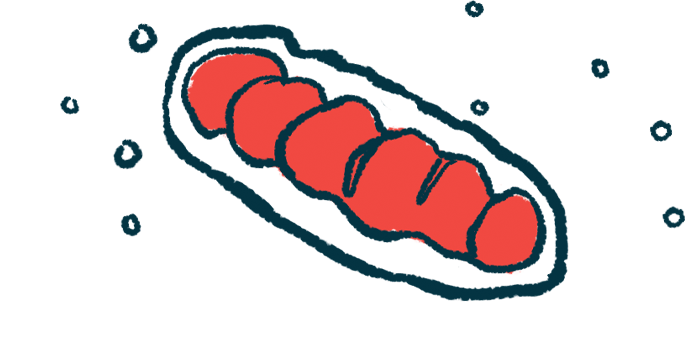
Mitochondria, cells’ powerhouses, have their own DNA that’s separate from the rest of the cell’s DNA. Cell-free mtDNA consists of mtDNA that’s released into circulation mostly from dying cells, making it a potential biomarker of cellular injury or stress.
“Our findings suggest that [mitochondrial] DNA dysfunction is a primary [disease] driver that precedes the full clinical manifestations of Parkinsonism,” the researchers wrote.
In Parkinson’s, nerve cells often show signs of mitochondrial dysfunction. As these cells need high levels of energy to function properly, mitochondrial defects may contribute to neurodegeneration.
Prior data have suggested that in Parkinson’s, this mtDNA, within neurons or circulating in bodily fluids, frequently has deletions, with chunks of the DNA sequence missing. These mtDNA deletions could contribute to mitochondrial dysfunction in Parkinson’s.
There’s been debate as to whether mitochondrial problems are among early changes causing Parkinson’s to develop, or if mitochondrial dysfunction occurs later on in the disease as nerve cells become damaged.
Sleep behavior disorder is known Parkinson’s risk factor
In the study, scientists analyzed cell-free mtDNA in cerebrospinal fluid (CSF) and blood from people with idiopathic REM sleep behavior disorder, or iRBD, which is marked by acting out vivid and violent dreams during sleep. REM stands for rapid eye movement, the phase of sleep in which most dreams occur.
The sleep disorder is a well-established risk factor for Parkinson’s and the related disorder Lewy body dementia (LBD). Both are characterized by accumulation of toxic aggregates of the alpha-synuclein protein. CSF is the fluid that surrounds the brain and spinal cord.
The study involved 51 people with iRBD. Of these, 34 later converted to full-blown Parkinson’s or Lewy body dementia, and 17 did not. Cell-free mtDNA levels in 20 similarly-aged people without iRBD or known neurodegenerative disease were analyzed as a control group.
Results from CSF analyses showed that iRBD patients, both converters and non-converters, had significantly more deletions in their mtDNA than the control group. Among those with iRBD, mtDNA profiles were similar regardless of whether they went on to develop Parkinson’s or Lewy body dementia.
The number of mtDNA deletions also tended to increase over time in people with iRBD. But in people with iRBD who went on to develop Parkinson’s or Lewy body dementia, mtDNA profiles were stable over the course of conversion: There wasn’t a notable uptick in mtDNA deletions when patients progressed from IRBD to full-blown Parkinson’s or LBD.
Further statistical analyses, adjusted for potential influencing factors, showed that the higher the number of cell-free mtDNA molecules with deletions in the CSF, the faster the conversion to Parkinson’s or LBD.
These findings support “the hypothesis that mtDNA dysfunction is a primary cause of neurodegeneration” rather than a consequence of nerve damage, the researchers wrote.
The data also suggest that mtDNA deletions measured in CSF could be a biomarker of the earliest stages of Parkinson’s-like disease, the researchers said.
The mtDNA analyses in blood samples didn’t show major group differences in deletion profiles. But levels of cell-free mtDNA in the blood were significantly higher in patients who went on to develop Parkinson’s or Lewy body dementia than in non-converters and controls.
“These findings suggest that quantification of [cell-free mtDNA] in [blood] may be of potential relevance as a blood biomarker of future conversion to” Parkinson’s or LBD, the researchers wrote, though they noted a need for further studies to verify and validate these correlations.
The study was funded in part by the Michael J. Fox Foundation.