Embryonic stem cell transplant showing safety in 12 patients
Treatment given in Phase 1/2a trial at low and high dose starting last year
A Phase 1/2a clinical trial evaluating TED-A9, a human stem cell-based therapy, in people with Parkinson’s disease has finished dosing with no safety concerns identified to date.
The therapy, delivered as a cell transplant directly into the brain, was given successfully to 12 adults diagnosed with Parkinson’s five or more years ago and with evident disease motor symptoms, according to its developer, S.Biomedics.
It is intended to directly address Parkinson’s underlying mechanisms by replacing the dopamine-producing nerve cells progressively lost to patients with precursor cells able to grow into healthy dopaminergic neurons.
Embryonic stem cell transplant as a way of restoring dopamine signaling
“TED-A9 could represent a fundamental treatment that surpasses current therapies, which only temporarily alleviate the symptoms of Parkinson’s disease,” Dong-Wook Kim, MD, PhD, TED-A9’s developer and chief technology officer of S.Biomedics, said in a company press release.
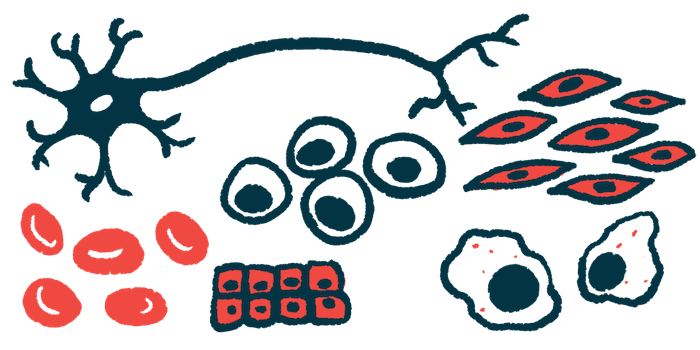
Parkinson’s symptoms are caused by the progressive loss of neurons that produce dopamine, a major chemical messenger in the brain, particularly in a region called the substantia nigra.
Much of the brain’s dopaminergic neurons reside in that region, with projections throughout reaching into areas such as the putamen, which is critical for motor control.
Approaches to restore or augment normal dopamine signaling in order to compensate for lost dopaminergic neurons are central to Parkinson’s care. But interest is increasing in the use of cell-based approaches that would replace the lost neurons.
Human embryonic stem cells, those found in a developing embryo, are self-renewing and pluripotent, meaning they have the ability to transform into virtually any type of mature cell under the right conditions. They are of growing interest as a potential treatment source for a wide range of diseases, including Parkinson’s.
TED-A9 contains dopaminergic progenitor (precursor) cells derived in the lab from these embryonic stem cells.
Transplanted into a patient’s brain, S.Biomedics expects that these cells will give rise to functional dopaminergic neurons, replacing those that have died off and helping to restore that person’s motor abilities.
“We have developed a fundamental therapeutic mechanism that directly replaces dopaminergic neurons lost in patients with Parkinson’s disease,” said Kim, who is also a professor in the department of surgery at Yonsei University in Seoul, South Korea.
The Phase 1/2a trial (NCT05887466), being conducted at that university’s hospital, enrolled 12 adults, ages 50-75, with Parkinson’s motor complications like freezing of gait, dyskinesia (uncontrolled movements), or off times despite being on a steady dose of a dopaminergic treatment like levodopa.
No safety concerns seen to date in treated patients, efficacy measures awaited
Six patients were treated with TED-A9 at a low dose (3.15 million cells) and another six received a high dose (6.3 million cells). The therapy was delivered via injections into the putamen during a single surgical procedure.
“The transplantation process targeted three segments of the putamen; the anterior, middle, and posterior sections, with three tracks per each putamen,” Kim said.
Safety will be monitored for a total of five years, and exploratory efficacy will be examined for two years using measures that include the Unified Parkinson’s Disease Rating Scale (MDS-UPDRS), Parts III and IV, which focus on motor symptoms, and a patient questionnaire of daily life quality.
To ensure treatment safety, an initial three patients were treated at low dose and monitored for three months before another three patients were treated at high dose and monitored. After no safety concerns, including dose-limiting toxicities, were identified in either group for those three monitoring months, the other six patients were enrolled and treated at low and high dose.
“The first administration began last year and completed the transplantation of 12 patients in February of this year without any special problems,” Kim said.
No side effects, complications, or unusual adverse reactions have been reported to date in these 12 patients following the transplant, according to the company.
The trial is expected to finish in February 2026.