Brain cells tied to REM sleep cycle, affected in Parkinson’s, identified
Fewer of these nerve cells seen in patients with REM sleep behavior disorder
Written by |
A specific population of nerve cells in the brain that helps to regulate REM sleep may be a key target for treating Parkinson’s disease, a study demonstrates.
REM (rapid eye movement) is the stage of sleep where the most dreaming occurs, with its other three stages classified as either light or deep sleep. REM sleep is essential for brain health, playing vital roles in allowing the brain to process and store memories. During normal REM sleep, the brain has a lot of electrical activity, but the rest of the body is essentially paralyzed.
“We identified a particular subtype of neurons that regulates REMS/[non-REMS sleep] and muscle atonia during REMS,” the researchers wrote, noting possible links between this cell population and some defining Parkinson’s characteristics.
The study, “A pontine-medullary loop crucial for REM sleep and its deficit in Parkinson’s disease,” was published in Cell.
REM sleep behavior disorder can be an initial sign of Parkinson’s disease
Problems with sleep are a common feature in Parkinson’s disease. In particular, many patients experience REM sleep behavior disorder, or RBD, a condition in which people act out their dreams during REM sleep, often with violent or erratic movements. RBD is often one of the first nonmotor symptoms of Parkinson’s, and it can appear long before the development of disease motor symptoms.
Although scientists have known about REM sleep since the 1950s, it’s still unclear exactly why REM sleep happens or what goes wrong in the brain to cause RBD.
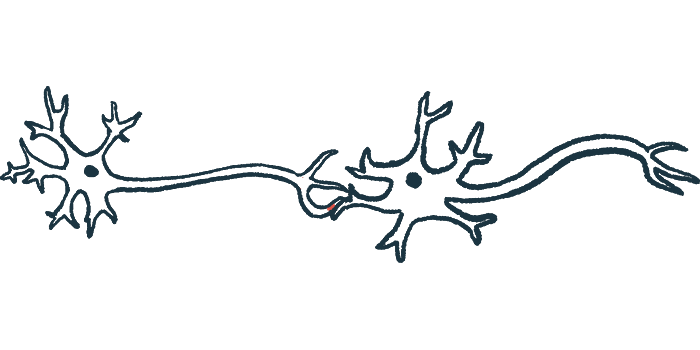
Through a series of experiments in mice, scientists largely in Japan discovered a unique set of neurons, or nerve cells, that seem to be essential for controlling REM sleep. These neurons are located in the brainstem (the bottom of the brain) in a specific region called the pontine sublaterodorsal tegmentum or SubLDT. The REM-regulating neurons can be identified because they express a particular protein marker called CRHBP.
Researchers found that when these CRHBP-positive neurons in the SubLDT are activated, mice were much more likely to enter into REM sleep, and they tended to stay in REM sleep longer. Conversely, when these neurons were damaged or inhibited, the mice spent much less time in REM sleep, and they also tended to move around more during REM sleep — which is very similar to what happens in Parkinson’s patients with REM sleep behavior disorder.
Nerve cells lacking in patients with RBD, but toxic alpha-synuclein evident
Building on this discovery in mice, the researchers examined brain samples from people with Parkinson’s and RBD, as well as samples from people without Parkinson’s for comparison. They found that the Parkinson’s samples had significantly fewer CRHBP-positive neurons in the SubLDT.
“These results strongly suggest that impairment of [CRHBP-positive neurons in the SubLDT] contributes to RBD and other sleep-related symptoms” in Parkinson’s, the researchers wrote.
At the molecular level, a cause of Parkinson’s is the buildup of toxic clumps of the protein alpha-synuclein in brain cells. The research team also noticed that CRHBP-positive neurons in the SubLDT of Parkinson’s patients showed high amounts of toxic alpha-synuclein buildup. Based on this observation, plus the fact that REM disturbances are often one of the first signs of Parkinson’s, the scientists said that these neurons “might act as an entry point for subsequent brain-wide propagation of [alpha]-synuclein.”
Turning back to mice, the researchers found that activating the CRHBP-positive neurons led to fewer REM sleep abnormalities in a model of Parkinson’s disease — implying these nerve cells might be a useful therapeutic target.
“Taken together, [CRHBP-positive neurons in the SubLDT] might be a target for ameliorating [Parkinson’s] progression,” the scientists concluded.