Blocking IL-6 release may rescue dopamine-producing nerve cell loss
In Parkinson’s, reactive astrocytes secrete high levels of neurotoxic molecule
Suppressing astrocytes’ release of the pro-inflammatory molecule interleukin (IL)-6 reduced the loss of dopaminergic neurons, the nerve cells that are progressively lost in Parkinson’s disease, a new study reports.
In Parkinson’s, astrocytes, the star-shaped cells that provide physical support for neurons in the brain, secrete high levels of IL-6 that exert neurotoxic effects on dopaminergic neurons. Halting the uptake of IL-6 by these neurons with tocilizumab, an FDA-approved antibody that blocks IL-6 signaling, eased their loss.
By finding “the right way to modulate the immune system, we could slow down the process of this disease,” Antonella Consiglio, PhD, at the Institute of Biomedicine of the University of Barcelona, Spain and the lead author of “Blocking IL-6 signaling prevents astrocyte-induced neurodegeneration in an iPSC-based model of Parkinson’s disease,” said in a university press release. The study was published in JCI Insight.
Parkinson’s disease is driven by the loss of nerve cells — known as dopaminergic neurons — in a brain region called the substantia nigra. These cells produce dopamine, a neurotransmitter needed for coordinating muscle movement. Neuroinflammation further exacerbates nerve cell death.
While astrocytes help regulate the brain’s immune system, studies on postmortem brain tissue from Parkinson’s patients revealed the presence of reactive astrocytes, which produce large amounts of inflammatory molecules.
Most Parkinson’s cases are of unknown cause, or idiopathic, but about 5% have a genetic origin, with mutations in the leucine rich repeat kinase 2 (LRRK2) gene being the most frequent known cause of late-onset Parkinson’s, where symptoms appear after age 50. When mutated, the gene halts the ability of the LRRK2 enzyme to elicit the breakdown of toxic material in nerve cells.
High levels of IL-6 cytokine
In Parkinson’s disease, high levels of LRRK2 activity have been found in both adaptive and innate immune cells, such as microglia and astrocytes.
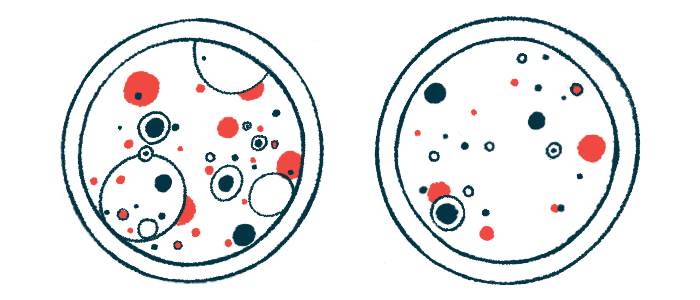
“These findings position LRRK2 as an essential player in controlling innate immune inflammatory pathways,” wrote researchers in Spain who generated astrocytes from induced pluripotent stem cells (iPSCs) from patients with late-onset or idiopathic Parkinson’s disease. Astrocytes derived from iPSCs corrected for the LRRK2 mutation, called an isogenic control, and healthy people were used as controls. IPSCs are derived from either skin or blood cells that have been reprogrammed back into a stem cell-like state, which allows for an unlimited source of almost any type of human cell to be developed.
When compared to control astrocytes, those from late-onset Parkinson’s patients expressed high levels of markers from reactive astrocytes. Moreover, these cells showed an altered expression of inflammatory molecules, called cytokines, and immune-related genes, which may contribute to disease progression.
A specific pro-inflammatory cytokine, IL-6, was released at higher levels from Parkinson’s astrocytes than from healthy and isogenic controls.
Adding a LRRK2 inhibitor for a week to Parkinson’s astrocytes prevented their reactivity and also significantly reduced the release of IL-6. Other pro-inflammatory and immune signals were also curbed by the inhibitor. The findings support that the activation of neuroinflammation in late-onset Parkinson’s astrocytes is mediated by LRRK2.
Next, in vitro studies revealed that exposure to culture medium from astrocytes derived from Parkinson’s patients triggered the death of neurons positive for tyrosine hydroxylase (TH), a marker for dopaminergic neurons. No effect was seen with medium from control astrocytes.
The degeneration of nerve cells was induced by the IL-6 released by astrocytes, since when researchers added tocilizumab, an antibody that blocks the IL-6 receptor, the number of living dopaminergic neurons was markedly increased. Tocilizumab, sold as Actemra among others, is approved for inflammatory conditions such as rheumatoid arthritis.
“It’s important to stress that the treatment of neuronal cultures with tocilizumab, an antibody that is already used daily in the hospital to treat rheumatoid arthritis and which blocks the effect of IL-6-secreting astrocytes, largely prevents nerve cell death”, said Manel Juan, immunologist at the Hospital Clinic de Barcelona and a study co-author.
Parkinson’s dopaminergic neurons were also more susceptible to IL-6-induced death than nerve cells from controls.
Testing the neurotoxic potential of IL-6
The researchers then assessed the reactivity and neurotoxic potential of astrocytes from patients with idiopathic Parkinson’s. iPSCs-derived astrocytes from three patients confirmed their reactive presentation and the release of IL-6 when compared with control astrocytes.
Like what was seen with astrocytes from late-onset Parkinson’s, IL-6 in the culture medium of astrocytes from idiopathic patients induced the death of dopaminergic neurons, which was eased by blocking IL-6 signaling.
These findings reinforced the idea that “IL-6 is one of the major mediators of astrocyte-dependent neurotoxic factors that play a role in the” progression of Parkinson’s, wrote the researchers, who also analyzed postmortem substantia nigra samples from Parkinson’s patients at early and late stages of the disease, as well as healthy controls.
Consistent with the lab studies, the activity of IL-6 was already detected in astrocytes of early stage Parkinson’s patients, with its expression significantly increasing from 2.62% in controls to 44.54% in early Parkinson’s to 56.86% in late Parkinson’s.
Indeed, even at the disease’ early stages, the susbtantia nigra showed much higher levels of IL-6 receptor expression than controls, “supporting the concept that reactive astrocytes producing elevated IL-6 levels and neuronal susceptibility to IL-6 play roles during [Parkinson’s disease] pathogenesis [disease progression],” the researchers wrote.
“Although the mild inflammation can be beneficial for many neuronal processes, the overproduction of IL-6 can worsen the symptoms of Parkinson’s disease, and this may be an important therapeutic target,” said Meritxell Pons-Espinal, of the University of Barcelona and the study’s first author.