A Preliminary Look at the Parkinson’s Disease Spectrum
Written by |
(Graphic by Dr. C)
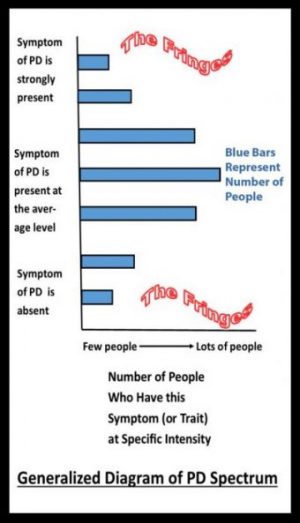
The needs of each Parkinson’s disease (PD) patient varies because there is a large symptom diversity in the disease population. We may think of this diversity as a Parkinson’s disease spectrum: some people display little or no symptoms of a certain type while others describe those same symptoms as severe.
The spectrum is not yet fully defined. In this column, I offer suggestions for the spectrum’s definition and discuss how it may help patients and medical providers. There are six parameters in the PD spectrum I’ve conceptualized. If measured in a clinical evaluation, the spectrum could help us better understand the disease.
Professionals have divided the disease into the “shaking type” and the “rigid type.” Patients from both types range in symptom severity. It is likely that these two types fall on a spectrum with shaking and rigidity overlapping each other in some patients. Let’s make tremors the first parameter, and rigidity the second.
Some PD patients have autonomic muscle involvement such as reduced blinking, urinary flow issues, and bowel movement problems. Let’s consider decreased functioning of autonomic muscles as the third parameter.
Interested in Parkinson’s Disease research? Sign up for our forums and join the conversation!
Patients also fall on a spectrum of nonmotor problems such as declining cognitive function, loss of emotive control, and sleep problems — the fourth parameter.
Not to make the whole thing overly complicated, but fifth and sixth parameters must be added to paint a decent portrait of the PD spectrum — the person’s history (pre-Parkinson’s brain and motor/nerve activity), and their current and past rehabilitation and treatment plan.
In summary, these six parameters could paint the Parkinson’s disease spectrum:
- Shaking symptoms (fine and gross motor) and associated pain/fatigue
- Rigid symptoms (fine and gross motor) and associated pain/fatigue
- Involuntary muscle changes
- Nonmotor problems (cognitive, emotive, sleep)
- Premorbid history (What was this brain used for? Includes nervous system, medical, and exercise histories)
- Current and past rehabilitation and treatment plan
I think all Parkinson’s patients should be evaluated using these six parameters. If we could hold in our minds these parameters and see that they paint a large spectrum landscape of PD diversity, then it may be possible to improve the quality of life for all those afflicted with PD.
I have an unusual form of Parkinson’s disease so I fall on the fringes of the spectrum (see the diagram). Not only is my disease mostly “invisible” but it also took quite a bit of medical sleuthing to arrive at the correct diagnosis. I went through more than a dozen doctors and an equal number of medications before arriving at Sinemet (carbidopa levodopa). The results were remarkable, and I am so thankful for that.
Being out on the fringes of the PD spectrum has created, and continues to create, problems which I’ll address in the columns to come. Knowing that I fit into the fringes made sense. I shared the spectrum and my place on it with others, which helped them understand my atypical form of PD.
Readers fit into the spectrum in different ways. They can say, “I don’t have that symptom, but I do have that one, and it’s the worst one for me.” Understanding that PD is a spectrum disease may ease the discomfort of symptoms being invisible to others. It can help to describe occurring symptoms to others, particularly your medical provider. It’s a challenge to find the words to match your experience, but the rewards are worth the effort.
Next week I’ll discuss a new look at freezing, called scenario looping.
***
Note: Parkinson’s News Today is strictly a news and information website about the disease. It does not provide medical advice, diagnosis or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or another qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website. The opinions expressed in this column are not those of Parkinson’s News Today or its parent company, Bionews Services, and are intended to spark discussion about issues pertaining to Parkinson’s disease.



David
Intriguing. Great that you respond to the classic Rx - not everyone does and certainly not consistently through their journey. Are there, then, pharmacotherapeutic sub-types? Pharmacokinetic?
Dr. C
Interesting idea - spectrum of medication responses - but outside of my realm of expertise. I am a rehabilitation therapist (RET), scientist, philosopher, and artist. I will do my best to confine my writing, including comments, to that which I have some level of qualifications.
Douglas Neslund
Dr.C, I am an adoptee (at birth), and also a Vietnam vet. I was diagnosed with PD at the VA as a result of Agent Orange exposure (as you likely were). Which calls a question to mind: is there a difference yet noted in the profession between those inheriting PD tendency, and those of us whose chemical exposures visited this disease on us? I am like you: Sinemet is doing a pretty good job of calming most tremors, and cervical cramping and curling toes are more recent events. Once in awhile, I will have an abdominal cramp that hits like a brick and is over with immediately (unlike the other cramping). I take a brain supplement that keeps me in the land of logic.
Pre-diagnosed health events include loss of smell/taste, bilateral retinal separations and subsequent treatments, loss of hearing on the affected left side of my body, occasional loss of normal left side vocal cord use (I teach voice, so I am aware of this), as well as prostate cancer (and loss of consortium, which the VA strangely does not consider a "disability"). I am rated disabled at 80%, but the tremor in my left side means piano playing (accompaniment while teaching voice) has rendered my employability as moot, which means I ought to be rated at 100%.
I ride a bike briefly and as furiously as often as I can, as well as raking leaves at this time of year, weather permitting. On the best days, my energy level tops out at about six hours; a bad day means napping and trolling the internet.
My sleep is unaffected, so far. I've always been a "thrasher" (restless legs syndrome) in bed, so that was probably inherited. As you mention above, most people don't see any symptoms, and believe me to be faking it, somehow. If they could only feel what the inside is doing all along the left side, from toes to scalp.
Thanks for your article.
Dr. C
I can relate to your story as their are some similarities to my own, in particular your mention of good days and bad ones. I will be doing a column on this in a few weeks.
Sachin
Hi I am a pediatric intensive care specialist working in Melbourne Australia. My father (now 80 yrs ) has symptoms for many years. We started him on medications last two years. Last 1 year, his symptoms are progressing rapidly (both motor and non motor). He is able to walk in straight line on plain surface. Direction change, initiating movement, complex movements are very difficult for him. He has lost bladder control. Agitation, restlessness, emotional lability very apparent. Speech has affected. Most of times , he is coherent and talks sensible but at times, he loses track of things and struggle to describe what he wants to say. I think his depression is playing major part in progression of symptoms rather than PD itself. He lives in India along with my mother and he feels very isolated, lonely. To what extent depression plays part in progression- anyone has any thoughts?? To what extent non pharmacological therapy- active/vigorous exercise, building up motivation, stimulating atmosphere, positive thinking play part in limiting disease progression. I will highly appreciate your thoughts.
Dr. C
Your dad sounds like he is struggling with the disease, as are family. It's tough on everyone. I have a column planned soon that will speak to a piece of depression (apathy), but depression is complex. There are many variations, causes, and symptoms. Sorting out the issues on depression, and other topics related to PD, is what I will hope to do a bit of in the columns to come. As for exercise - when matched to the person's situation - I think it is the one best thing to help people with PD. Best wishes to you and your family.