Managing Chronic Pain, Part 1: Understanding a Shift in Perspective
Written by |
Pain and suffering are not the same. An internet search for “difference between pain and suffering” yields dozens of sites for writers and practitioners, like Ashley Pennewill and Ann Marie Gaudon, who extol the benefits to be gained from this conceptualization. The repeated message is that pain is the physical experience connected to insult and injury, while suffering is the “story” we tell ourselves about the pain experience. Our total pain experience is the sum of physical pain and suffering, with each affecting the other.
Shifting my perspective on chronic pain to one that understands the role of suffering in the total pain experience has helped me to better manage my chronic pain (including discontinuing opioid treatment), decrease the occurrence of dysregulated emotions, and achieve an overall improvement in well-being.
The difference between pain and suffering is an encyclopedic topic that has been the focus of writings since at least the time of the Buddha. A focus on the mind-body link examines how we can use that information to reduce suffering so that we can better manage chronic pain.
The Parkinson’s Disease News Today forums are a place to connect with other patients, share tips and talk about the latest research. Check them out today!
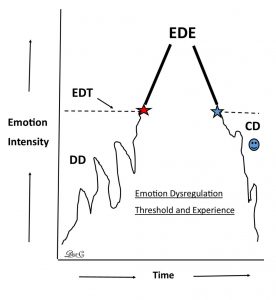
The mind/body link as an attention-to-stimulus process was partially described in my column on irritability. The process of pain stimulus creates the need for attention to the stimulus. The feelings and thoughts associated with the stimulus escalate. It is a feedback loop that helps us in the face of danger, but as the feedback cycles out of control, emotions often become unregulated and out of control. The spiraling loop can become a barrier to well-being. The experience of emotion dysregulation (see figure) is one link between the pain, feedback, attention processes, and suffering.
The figure illustrates emotion dysregulation as an experience connected to exceeding one’s emotion dysregulation threshold (EDT) due to increasing emotional intensity over time (dysregulation delay, or DD). Once the threshold is crossed, we experience emotional dysregulation (EDE). This is followed by a cooling of the emotion intensity (CD). The goal is to reduce the intensity and duration of the emotional dysregulation. This is where the shift in perception is applied.
It is a shift from feeling like we can’t do anything to keep our emotions from getting out of control to an understanding and belief that we can change the escalation. It is adopting the perception that we have some control over this dysregulation and that, given the nature of neural plasticity, there is the possibility of reducing the intensity of dysregulation experiences and lengthening dysregulation delay times. This success can lead to less suffering and make it easier to manage chronic pain.
Pain is reported by many Parkinson’s patients. “Among the different forms of PD-related pain, musculoskeletal pain is the most common form, accounting for 40%–90% of reported pain in PD patients,” according to a paper by Orjan Skogar and Johan Lokk.
“Individuals with Parkinson disease (PD) frequently suffer from pain that interferes with their quality of life but may remain under-recognized and inadequately treated,” reports Neurology Times, citing a study published in the Journal of Neurology. I am one of these individuals. I have good days and very bad days — the ugly days.
The Neurology Times article continues, “’We found pain to be highly frequent, quality of life-impairing but insufficiently and unsystematically treated,’ wrote first author Carsten Buhmann, MD, of the University Medical Center, Hamburg-Eppendorf (Hamburg, Germany) and colleagues.”
When we live with Parkinson’s and experience pain, we are not alone. The Parkinson’s Foundation says, “Chronic pain is twice as common among people with PD as it is in people without it. In fact, more than 80 percent of people with PD report experiencing pain and say it’s their most troubling non-motor symptom.”
I am in pain most of the time. I cross the threshold when I am having difficulty managing the pain and the connected feedback loop. If I add some additional stressor — emotional, physical, or situational — that feeds the emotional turmoil, and I cross the threshold sooner. Accepting that I can do something about it (and have the skills) is the shift in perspective. It is a shift from being a servant to the whims of my emotions and their consequences to presenting as a calm, centered being who seeks continued progress on his wellness map.
I am still learning and practicing techniques to help me shift my perspective so that I can manage my chronic pain more successfully. I will discuss some of these techniques in Part 2 of this series. Attempts to change human practices are only as effective as the intent behind them. The shift in perspective allows us to firmly establish this proper intent.
What are your thoughts about emotion dysregulation and human suffering? Please share in the comments below.
***
Note: Parkinson’s News Today is strictly a news and information website about the disease. It does not provide medical advice, diagnosis or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or another qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website. The opinions expressed in this column are not those of Parkinson’s News Today or its parent company, Bionews Services, and are intended to spark discussion about issues pertaining to Parkinson’s disease.



Chris Tay
Thank you for your contributions to the awareness of the mind/body link. I am in my 3rd year after atypical PD diagnosis and am trying to integrate the two. Perhaps the simplest form of this, I have dicovered, is in exercise. Your mind is telling your body "I am going to do something about this" as you jump on your bike. 30 minutes later, your body is telling your mind " That worked , I feel better!" This is establishing a positive feedback loop which, so far, seems to also help with depression and mild pain.
I look forward to your next article.
Dr. C
Hi Chris ~ I think it is wonderful that your mind/body connection is giving you the positive feedback loop experience. Exercise will help with the pain and the depression. Getting (and staying) motivated is essential. It does work and I agree with you that after a good workout "I feel better" too. I had PD confirmed diagnosis in 2014 and although I don't have the tremors (yet), I seem to have most of the other symptoms. Fortunately I'm able to exercise and find that it helps. I used to cycle years ago -- now I have an indoor exercycle that I will start using after gardening season ends. I feel safer using that instead of biking -- if I fall off, it will only be a short drop to the floor! Thanks also for encouraging words about the columns. I can't thank you and other readers enough, and all the good folks at BioNewsServices who support my writing.
Dr. C.
William Vance
Very good and helpful information. Keep it up
Thank you
Dr. C
Hi William ~ Thank you for the appreciation of my column and ideas. Your support and recognition means a great deal to me -- it's my reason to keep writing and sharing information.
Dr. C.
Garrett McAuliffe
I have tried to learn to separate discomfort from suffering by practicing mindfulness meditation. It works most of the time. Acceptance and commitment therapy is one method of doing that and I see a therapist who practices that approach. But I woke up this morning with symptoms – tremor plus anxiety – And I couldn’t quite find my way to the “it’s only my mind” Mindfulness. So the symptoms themselves to cause some anxiety inherently. And I try to separate those from catastrophizing I guess.
Dr. C
Hi Garrett ~ There are good days and bad days and then there are ugly days (see my previous column on this topic). Despite the best we can do, the symptoms get in the way sometimes. Threshold management is what I am trying to use in addition to accepting the moment -- and medication. Acceptance plus medication is not enough to deal with the bad and ugly days. What you have to add on to that is high self monitoring tied to threshold management. Basically it is a practice of listening to early precursor signs that indicate PD symptoms are revving up. When this occurs, I stop everything and take a quiet 10-15 minute deep meditation break. It doesn't work 100% of the time, and I may have to do is several times in a day, because I still have to deal with old ways that interfere in the process of dealing of new ways of threshold management. I am still trying to remove the "old ways" in dealing with threshold management. Threshold management is about high self monitoring and catching the surge before it becomes catastrophic. It is not an easy thing to do but it is possible.
Keep in touch... I love your posts!
Dr. C.
Christine
After 53 years I have recently rekindled a relationship with the love of my life who is a PD sufferer. I knew nothing about PD and am currently experiencing the steepest of learning curves. I so want to help him but feel that I am treading on egg shells in not knowing what I can say to him and how to say it. He copes so well and has never been sharp with me but I can see his stress and anxiety in his face/behaviour/tiredness and I know that I must respect his dignity at all times. He keeps himself very busy but struggles to walk away from what he is doing even though he knows this will stress and tire him. He also sets himself impossible goals and gets very upset when he fails to achieve them. How can I help him to break the cycle and walk away from his work at an appropriate time? I have spoken with him about it and it is almost as if it is beyond his control. He does occasionally do a 30 minute bike ride at the end of the day and says he feels much better after it. I really want to help but I worry that he'll think I am interfering too much.
Dr. C
Hi Christine ~ Welcome to Parkinsons News Today and thanks very much for reading my columns. Your comment sums up a lot of what Mrs. Dr. C. and I go through and have gone through with my Parkinson's. I've asked Mrs. Dr. C. to respond as she is integral in helping to manage my PD:
"Hi Christine -- this is Mrs. Dr. C. I think you so well describe the processes that we have been through. If you are in a relationship with someone who wants to be active, engaged and interact with the world, and who has PD, it can be a balancing act. Acknowledging the struggle is part of the communication process between you two. We have cueing systems for checking in on taking meds, noting the elapsed time on a project, or working hard on scheduling not so much in a day or consecutive days. Maintaining the dignity of your loved one is important but being the reminder person must also be accepted and acknowledged. It has taken quite a while for Dr. C. to accept that my check-in or reminders are not nagging but an effort to avoid what we both know can be a rapidly downward spiral physically, psychologically or emotionally if he overexerts. We write the columns together (I mostly edit and do the research for references while he lays down the "big picture"). We would hope that you and your partner would gain some useful information and insights in to what you describe as challenges most PD patients, and their loved ones, face. Perhaps sharing the insights from our columns, and those of the other writers here at Parkinsons News Today, will give you both some insight and some ideas. Above all, keep talking about what he and you are feeling, thinking, experiencing. It sounds like you have a strong foundation of love to build upon. ~ Mrs. Dr. C"