Devices to Record the Progression of PD
Written by |
The progression of Parkinson’s disease (PD) is unique to every person, with different early, middle, and late-stage symptoms. However, this view of PD progression may be an artifact of limited data rather than an accurate description. We need new ways of measuring PD symptoms as they change over time. We have the technology to create new devices that people can use over an extended period, across multiple settings and severity of “off periods.”
I see progression as a change in the intensity and duration of “bad” days and off periods. Many longitudinal studies investigate the progression of PD (for example, the rate of progression in exercise), but it is hard to find studies that measure changes in response to treatment. Devices discussed in this column might change that.
Better measurement of PD progression begins with a few assumptions. First, subtle, early motor symptoms will appear before more obvious symptoms, such as tremors or bradykinesia. Second, early motor symptoms will be inconsistent and episodic. Third, we have the technology to build mobile monitoring devices.
I recently read that a patient being evaluated for “internal tremors” showed no signs of tremor during a physical examination of his bare feet. However, once he put his socks and boots on, an astute clinician observed the left bootlace swinging in such a way that, when measured, fit the PD pattern of a tremor. In other words, while the patient didn’t exhibit tremor during a visual examination of his bare feet, his shoelace reflected an underlying tremor!
A shoelace is not going to be a reliable measuring device, but it proves that slight motor changes that are difficult to detect do exist. I’ve designed two possible motor symptom detection devices: a mobile swing monitor (MSM) and a fine motor skills test (FST). Both devices would record and monitor movement fluctuation over time and across settings in daily life over 10 or so days. Both devices use sensors to track and record movement through three dimensions.
The MSM uses five “movement in 3D space” sensors — one on each wrist, one on each ankle, and one on the belt — with recording hardware for all five. Worn for several days, like a Holter monitor, the MSM would map the sway of the arms, legs, and body over time and across settings. The MSM is very similar in appearance to wearable training weights, which can measure the slightest variations in body movement. Wearable training weights are used by Olympic and World Cup judges to evaluate Shaun White’s amazing snowboard flips and twists.
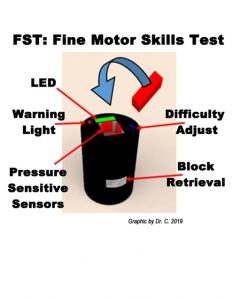
The FST, illustrated in the graphic below, has a 3D monitor in the “soda can” receptor where the block is inserted. Similar to the game “Operation,” the patient must remove objects from openings in the receptor without setting off the buzzer. The warning light goes off when the sensor plate is touched.
The FST will measure how the person adjusts position and control while using fine motor skills. The FST uses a 3D monitor and four independent, pressure-sensitive plates that record when the patient fails to insert the block and when the block is aligned. The plates can be positioned at different widths using an adjustable difficulty setting, making it harder to insert the block without touching the plates.
Data gathered by these two devices may provide patients and medical professionals with more accurate clinical data about motion, tremors, and fine motor skills over a greater period. They could demonstrate the progression of intensity and duration of bad days and off periods and serve as the beginning of a database on PD progression.
Many people are excited about using technology to provide outcome measures. As we know, technology is not being utilized in offices with patients to help understand the progression of PD. But hopefully, that will change.
If these devices are already being tested in the home of PD patients, sign me up!
***
Note: Parkinson’s News Today is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or another qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website. The opinions expressed in this column are not those of Parkinson’s News Today or its parent company, Bionews Services, and are intended to spark discussion about issues pertaining to Parkinson’s disease.



Teresa Prego
Hello Dr. C,
Wanted to reach out, to let you know that PKG®, which measures and reports movement symptoms of Parkinson's, and creates a report for clinicians to better understand what's happening in the day to day life of a person with Parkinson's, is currently being used in the US. It is a wrist-worn sensor that collects movement data over the course of 7 days that is then run through an algorithm to generate a summary report. We're interested in connecting with individuals like you, to better understand how best to enable optimized sharing of information between people with Parkinson's, caregivers, and clinicians. Please feel free to reach out if you're interested in further conversation! [email protected]
Dr. C
Hi Teresa ~ Thanks for the information in your comment. I will contact you directly to continue the conversation. I am very pleased that you read my column and felt it pertinent to the device you mention.
To my readers -- Stay tuned, as I explore this in more detail!
Dr. C.