Deep brain stimulation surgery was life-changing for my husband
DBS helped Eric find relief from his most debilitating Parkinson's symptoms
Written by |

I’ve often heard people scoff “It’s not rocket science” or “It’s not brain surgery” when expecting someone to accomplish an easy task.
But as I tried to calm my jangling nerves, an important clarification ran through my mind: “This is brain surgery.”
I was alone with my thoughts in the hospital waiting room after my husband, Eric, had been taken back for deep brain stimulation (DBS) surgery. He’d been prepped by his neurologist, neurosurgeon, surgical team, and a representative from Boston Scientific, a medical device manufacturing company. I’d sent him off with a quick kiss, and then he was wheeled into the operating room for the first of two DBS surgeries to treat his advancing Parkinson’s symptoms.
That was two years ago, but I remember it like it was yesterday. A neurologist diagnosed Eric with Parkinson’s in 2014. Over the next eight years, the disease progressed, but Eric’s symptoms were never tremor-dominant like so many other people with Parkinson’s. His version of the disease manifested as extreme joint stiffness, muscle rigidity, bradykinesia (slow movements), and dystonia, which presented as a constant, painful writhing and cramping of Eric’s feet that made his toes curl and twist. He also complained that the pressure on his shoulders felt like an anvil pressing down on him.

Eric Hammergren’s incision after DBS surgery No. 1. (Photo by Jill Hammergren)
Medications helped with various symptoms, but his off times had become horrendous — especially the crawling. Tears quickly fill my eyes when I recall those horrific images permanently seared in my memory. When Eric couldn’t get his dopamine-depleted brain to move his body, he dropped to all fours and crawled. Seeing the hopeful strides of babies exploring independently on their hands and knees may be awe-inspiring. When a man in his 60s is forced to crawl by the stranglehold of a neurodegenerative disease, it’s demoralizing and dehumanizing. As the woman who loves him, experiencing these excruciating moments left me devastated and helpless.
Eric’s neurologist was confident that bilateral DBS would improve Eric’s long-term quality of life with Parkinson’s. We were more than ready to try it.
The long process
Preparing for and undergoing DBS surgery was a process. Psychologists gave Eric several cognitive tests to determine his tolerance for surgery. During an office visit a week before the first operation, the neurosurgeon drilled four anchors into Eric’s skull and then sent him for an MRI. This would help the team map the size and shape of Eric’s brain and the anchor locations so a halo brace could be customized and anchored for surgery. Imagine something similar to a round locking anchor on ready-to-assemble furniture. The anchors didn’t protrude like the bolts on Frankenstein’s monster, but they were visible in Eric’s head for a week.
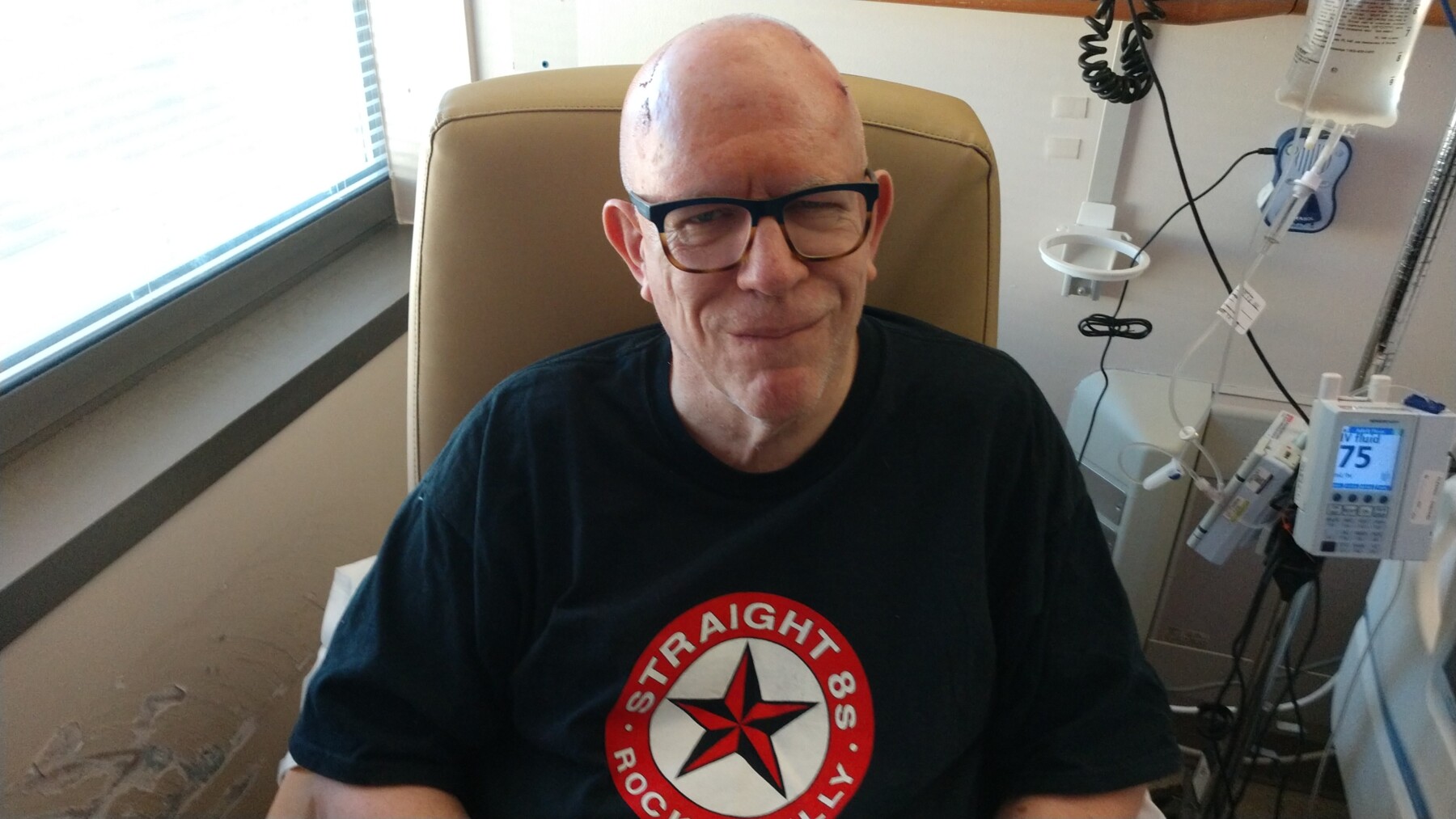
Eric Hammergren smiles after his first DBS surgery. (Photo by Jill Hammergren)
Eric had to stop taking his Parkinson’s medications 24 hours before the first surgery. He was miserable and couldn’t function well. I struggled to get him out of the house and into the car for our predawn ride to the hospital. Our emotions were raw and strained. In total, Eric went 36 hours without his meds. We then struggled to have them administered on a rigid schedule in the hospital. As a caregiver, I had to relentlessly advocate for Eric’s needs.
Eric and his neurologist selected a DBS system with two flexible wire leads that enabled the doctor to target very specific areas within Eric’s brain near the substantia nigra, a part of the brain that produces dopamine and helps to control body movements. The system’s stimulator has a 15-year rechargeable battery.
Here’s a remarkable note: The surgical team kept Eric awake during the four-hour surgery so he could help them determine which placement would be most effective in alleviating some of his Parkinson’s symptoms.
I thought I was prepared to see the big, curved incisions across the top and side of Eric’s bald head, but it was still shocking. However, his smile was wonderful.
During the second surgery a week later, the neurosurgeon tucked the wire leads behind Eric’s right ear and down through his neck, and then hooked them to the neurostimulator he implanted in Eric’s upper right chest, just below his shoulder. The stimulator is akin to a pacemaker, but this device keeps Eric’s brain stimulated night and day.
A month later, the neurologist used a portable tablet to access and program Eric’s DBS system, and it can now be adjusted as needed. Eric uses a remote to change the settings, and he charges the device weekly by sitting with a sleeve that holds the charger atop the stimulator in his chest.

Eric Hammergren shows the incisions on his head and chest after his second DBS surgery. (Photos by Jill Hammergren)
DBS has been a life-changing experience for us. It alleviated some of Eric’s most bothersome Parkinson’s symptoms and enabled him to eliminate three medications. Eric still struggles with the roller coaster of off times and some gait freezing, but we are thankful for advancements in technology and ongoing Parkinson’s research.
Note: Parkinson’s News Today is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or another qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website. The opinions expressed in this column are not those of Parkinson’s News Today or its parent company, Bionews, and are intended to spark discussion about issues pertaining to Parkinson’s disease.





Marjorie Weiss
My husband had deep brain stimulation surgery in 2007 for the left side of his brain on 2009 for the right side of his brain. He continues to receive benefit from them even after all these years. His surgical steps were a bit different but overall much the same. I wanted to post this so people could see the hope that comes with his getting relief from his parkinsonianisms for this long of a period.
He has had Parkinson’s for more than 20 years having been diagnosed in his early 50s. He continues to be able to walk with no assistance and has very little tremor and does not need much medication. He participates in rock steady boxing and exercises regularly. He has also been trying to B1 therapy
Jill Hammergren
Marjorie, it's great to hear that your husband has benefited from his DBS for a long time. That's very encouraging for us and for others considering the procedure.
Laurie
My husband underwent DBS surgery yesterday. He is only 57 and his quality of life wasn’t great due to his Parkinson’s tremors and dyskinesia from Parkinson’s meds. I did not find his medications helped much with his tremors. I am here with him at the hospital not ever 24 hours after his procedure and although he is awake, he is responding with one word only to the nurse and he is ignoring me completely. I know it is early and that this procedure was a lot of stress on his body. Just wondering if this is normal. I am hopeful his quality of life improves for many years to come. It is great to hear about your husband’s successful outcomes.
M Nicholson
This is so encouraging for all those who are considering DBS. For those of us who do not live in less developed counties (where the procedure is not available ) and/or have no medical insurance, some idea of the cost would be helpful
Vickie Kapp
I have been thinking about DBS for several years now, but too scared to go forward. I am 70 yeas old, was diagnosed at age 55 in 2008, and I am generally in good health.. My most bothersome symptom is dyskenisia, which is unpredictable, sometimes painful, and exhausting. I also experience unpredictable off periods, balance, and gait issues. What helped other PD sufferers like me, make the decision to have the surgery? How were the results of your surgery? Did anyone have a bad or disappointing result from DBS surgery, and wish you didn't have the surgery?