Overactive dopamine cells may drive Parkinson’s brain damage
Neurons in substantia nigra are hit harder than cells in other parts of brain

Brain damage in Parkinson’s disease may be driven in part by certain nerve cells working too hard, causing them to accrue damage and die. This suggests that treatments that reduce the activity of these cells may help slow the brain damage that drives the condition.
That’s according to the study, “Chronic hyperactivation of midbrain dopamine neurons causes preferential dopamine neuron degeneration,” which was published in eLife.
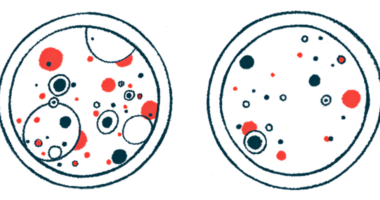
In Parkinson’s, the brain cells that produce the signaling molecule that nerves in the brain use to communicate with each other, called the dopaminergic neurons, become dysfunctional and die. Dopaminergic neurons in the part of the brain called the substantia nigra, which is essential for controlling movement, are usually hit harder than the dopamine-making cells in other brain regions. This pattern of nerve damage is an established hallmark of the disease, but it’s not clear exactly why these cells are more vulnerable to Parkinson’s-related damage.
“An overarching question in the Parkinson’s research field has been why the cells that are most vulnerable to the disease die,” Ken Nakamura, MD, PhD, co-author of the study at the Gladstone Institute for Neurological Disease in California, said in an institute news story. “Answering that question could help us understand why the disease occurs and point toward new ways to treat it.”
Research suggests that, in Parkinson’s, the dopaminergic neurons in the substantia nigra are actually more active than normal, meaning the nerves’ overactivity may contribute to disease-driving damage.
Do overactive neurons cause Parkinson’s
In this study, Nakamura and his colleagues genetically engineered mice so their dopaminergic neurons would be more active when exposed to a chemical called clozapine-N-oxide (CNO) to test whether increasing the activity of these nerve cells is enough to cause Parkinson’s-like damage.
“In previous work, we and others have transiently activated these cells with injections of CNO or by other means, but that only led to short bursts of activation,” said Katerina Rademacher, a graduate student in Nakamura’s lab and first author of the study. “By delivering CNO through drinking water, we get a relatively continuous activation of the cells, and we think that’s important in modeling what happens in people with Parkinson’s disease.”
Soon after the mice started being given CNO, dopaminergic neurons in their brain began to show damage and die, with dopamine-making cells in the substantia nigra showing much more damage than similar cells in other brain regions, which is what happens in Parkinson’s.
This suggests dopaminergic neurons in the substantia nigra are especially vulnerable to damage from being too active. One explanation for this is that these nerve cells have “immense energetic requirements,” said the researchers, nothing that “even mild hyperactivity may trigger or accelerate degeneration” in these cells.
They suggested that, in Parkinson’s, there may be a vicious cycle wherein some dopaminergic neurons in the substantia nigra die, forcing the remaining cells to work harder, which drives more damage and leads to even more cell death.
“If that’s the case, it raises the exciting possibility that adjusting the activity patterns of vulnerable neurons with drugs or deep brain stimulation could help protect them and slow disease progression,” Nakamura said.