‘Bananas and Beans, not Burgers’: High-Protein Meals and Levodopa
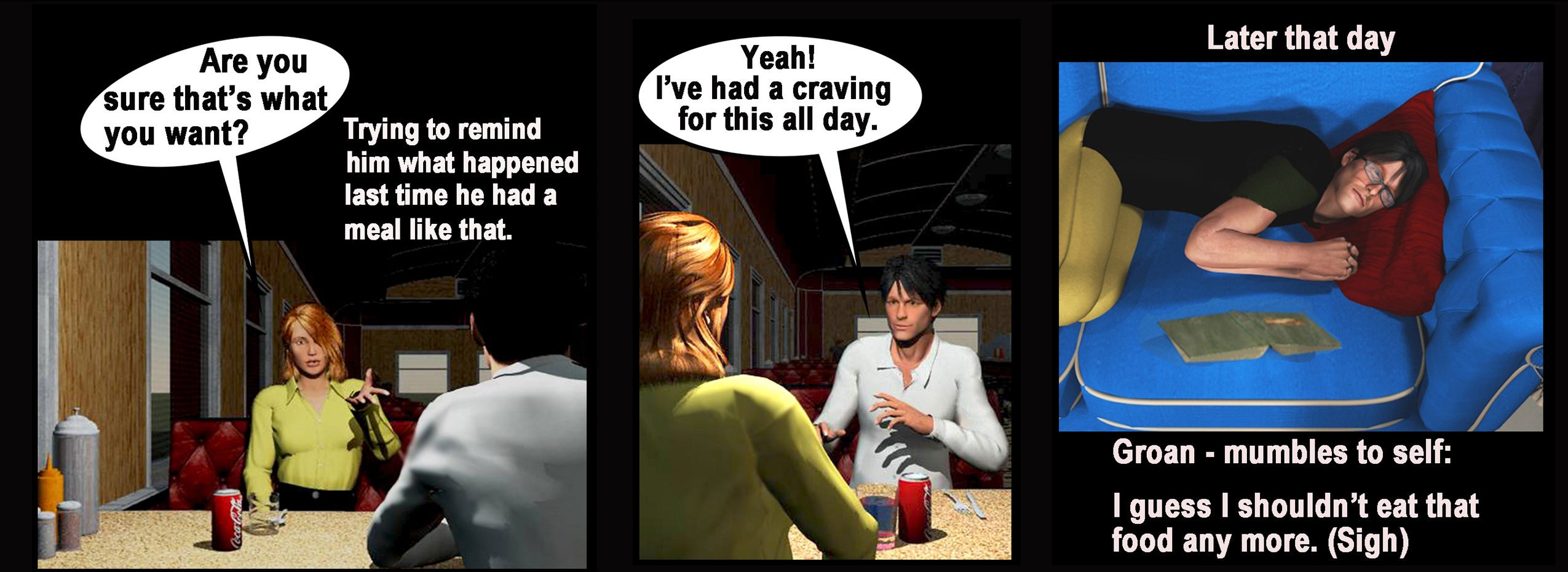
(Graphic by Dr. C)
No one told me that breakfast bacon, ham, or sausage would make me feel awful!
I had seen my off-periods worsen after a heavy meat meal, but I shrugged it off as “just a bad off-period.” Now, after being on levodopa for five years, I am positive that animal protein meals are a serious issue. Overlapping a high meat meal with levodopa can result in not just an off-period, but also one that lasts much of the day.
“Bananas and beans, not burgers” is the mantra to remind me that diet is very important in the development of a rehab plan for folks with PD. I am not a nutritionist. I am writing from the perspective of a PD patient warrior and rehab clinician.
Research suggests that changes to your diet could help alleviate some symptoms of your PD. The American Parkinson Disease Association (APDA) notes that levodopa crosses the wall of the small intestine via molecules in the intestinal wall that transport amino acids. When dietary protein (beef, chicken, pork, fish, eggs, nuts, and dairy) is also present in the small intestine, fewer transporters are available for levodopa to use. We may experience the “protein effect” when the medication competes with a high-protein meal.
One of the most compelling statements in a 2014 study published in Frontiers in Aging Neuroscience is that a “growing body of evidence suggests that nutrition may play an important role in PD.”
The study “Irregular gastrointestinal drug absorption in Parkinson’s disease” in the journal Expert Opinion on Drug Metabolism & Toxicology states that levodopa transit time in the small intestine is approximately three hours. Therefore, gastric emptying is a major determining factor for the onset of symptom relief. When PD delays gastric emptying, it has the potential to cause motor fluctuations, known to us as off-periods.
The Parkinson’s Disease News Today forums are a place to connect with other patients, share tips and talk about the latest research. Check them out today!
Research also shows that with your microbiome (the microorganisms in your body), a relationship exists between Parkinson’s disease and improved gut health. In “Parkinson’s disease and bacteriophages as its overlooked contributors,” published in the journal Scientific Reports, George Tetz and his colleagues examined the viruses that live in the gut, as well as the role the microbiome may play in Parkinson’s disease. According to Parkinson.org, “this has sparked the idea that we might be able to improve the symptoms if we change the microbiome through diet or other ways. … These bacteria play a role in the processes that produce dopamine and affect the intestine’s ability to absorb.”
Like many aspects of Parkinson’s symptoms, the protein effect is highly variable. Some people do not experience it at all. Others are extremely sensitive to protein’s effect on medication absorption. This diet concern was presented at my local PD support group, and the group’s PD warriors and caregivers agreed almost unanimously with having experienced or witnessed the adverse effects.
It typically becomes more of an issue as PD progresses. The APDA suggests that if someone experiences the protein effect, two potential strategies might help. One is to refrain from eating protein during the day, eating it at night instead, when the medication’s effect is less critical. The second is to distribute protein intake evenly throughout the day so that medication absorption is enhanced during that time.
The solution I have found that works best for me has two parts. First, I space the levodopa dosing so that it occurs between meals to minimize absorption issues. Second, I eat the day’s moderate meat meal at lunch, not dinner or breakfast.
Reducing meat in your diet may be beneficial not just to levapoda absorption. An amazing study on diet and overall health by Thomas Campbell and T. Colin Campbell, called “The China Study,” clearly showed that decreasing meat intake is a good change for all of us. Bananas and beans, not burgers.
What diet changes have you found to be helpful? Share in the comments below.
***
Note: Parkinson’s News Today is strictly a news and information website about the disease. It does not provide medical advice, diagnosis or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or another qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website. The opinions expressed in this column are not those of Parkinson’s News Today or its parent company, Bionews Services, and are intended to spark discussion about issues pertaining to Parkinson’s disease.







Thanks for this article. I have long been a believer that diet plays a crucial role in everyone's health, even those without PD. I have been a vegetarian for over 10 years (mainly for animal welfare reasons), Within the past year I have tried to eliminate cheese and dairy, try to be gluten free and avoid sugar if my addiction doesnt overwhelm me. LOL
What are your thoughts on sugar, dairy and gluten (often considered inflammatory) and impact on PD? I plan to get my CRP level (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4517917/) tested for a baseline. hen be very strict with my diet (NO dairy, sugar or gluten) for 6 months and then see how I test.
Dr. C.
I also have high sensitivity to gluten and lactose products. I've eliminated almost all from my diet for years. My only "addiction" is Ben and Jerry's ice cream which I avoid as long as I can and then usually enjoy as a "treat". Chocolate is another nemesis. But sugar and chocolate don't seem to have the same detrimental effects on my PD symptoms as protein does. I've mentioned the protein:PD connection to several neurologists -- all of whom denied the correlation. It was one of my first symptoms, before even starting levadopa, that I would "crash" after a protein-rich meal.
R. Mack
Thank you for publishing this article about the negative interactions between protein and levadopa.
I am a healthy, youngish-senior woman, and have been taking medication for and dealing with the challenges of PD for 12 years.
I was diagnosed with PD in 2007 and by 2013 had found that I had much worse off-times after eating meat. I cut my consumption of meat drastically, and found a huge benefit in shorter, less adverse off-times, but I could still enjoy chicken and fish for some time. It is always a struggle to balance medication times and meal times to avoid off-times, but reducing my protein consumption made a positive difference. Over the past 6 years, time marched on and in order to enjoy life as much as possible, I now control my protein intake to less than 10 grams per meal, whether it is animal, fish, eggs, or plant-based, and, for me, spacing protein throughout the day has proven to be my best option.
Dr. C.
See my comment to Jean Mellano. I agree with your observations that balancing the protein/PD symptoms/medications can be a challenge. I am on mostly plant-based protein now. Occasionally I'll indulge in some thin-sliced chicken or turkey or tilapia. Gave up salmon because it was too "heavy" even for fish protein. Most of my dietary changes were self-administered. I have yet to find any neurologist who believes that a dietary consult should be a standard practice for patients with PD. Good work on your self-care and lifestyle changes.
Teresa Binstock
I have found that meat protein is like a lump in the gut. Salmon included. A 2006 WebMD summary of diet (not just for PD) is merits contemplation.
Dr. C
I agree -- meat protein does a number on my PD. Instant off cycle! In fact, it was one of the first indications of non-motor PD that I had. Took me several years to understand that the great egg and bacon and sausage breakfast at Denny's was making me almost comatose. I've had to give up salmon and other oily fish protein as well. "Nuts, roots and berries," as my wife refers to our diet. Unfortunately most neurologists I've talked to have no idea or are adverse to the idea that protein interferes with PD.
Thanks for reading the column and I appreciate you sharing your insight and experience with one of the challenges we all face.
Dr. C.
Dwight
I've been searching the web to find someone else struggling with a very significant negative response to levopopa absorption with eating protein. Diagnosted 17 years ago, DBS in years 8 and 10 have made life miraculously better. Turn off stimulators and I turn into a rock...no exaggeration.
However, eat a lot of pizza (love it) for a couple of days and I'll have serious stiffness/slowness for a couple of days afterwards. I've actually been on juice fasting diets for multiple days and feel better as time goes on (up to 5 days). Just finally starting to work with food nutrition expert, I'm concerned about impact of too low of protein over time.
Is there anyone else out there dealing with such an extreme situation?
Dr. C
Hi Dwight ~ You describe your observation well. I have the same problems. In fact, it was one of the early symptoms that I experienced that led me to seek an answer of what was going on with my body. I didn't expect to find out it was the Parkinson's. I could eat a big breakfast -- eggs, sausage, hash browns -- I would be unable to move, my muscles would tighten up and it would take hours to return to "normal". There are many scientific studies that indicate that concentrated animal protein does interfere with the dopamine release process. Over the last 6 years I have amended my diet habits to eat eight small meals throughout the day. I will have one egg in the morning for breakfast or occasionally a miniscule portion of chicken or turkey sausage. I snack on small protein supplements, not sugar. Beans and legumes are a part of my diet to help supply non-animal protein. I probably love pizza as much as you do -- but with gluten-intolerance and dairy-intolerance the combined experience is absolutely wretched. If I don't follow my plan then I feel terrible, but every once in a while I do enjoy a trip to KFC or Dairy Queen to just take a break from my diet protocols.
Dr. C.
Jo Starno
I feel better now- after reading this article that is. I am not imagining how I feel after eating meat or dairy products, like my dr thinks! None of her other patients have this problem, so she told me.
It seems that if drs have not read something in a medical journal it doesn’t exist! That’s sooo comforting for the patient to have their symptoms negated by their medical provider. (Yes, I have experienced this in my quest for health care with Parkinson’s.)
At any rate, - the search for better treatment, better drs & eradication of Parkinson’s goes on. Patients have to be their own advocates & make sure they are receiving the best possible care available in this disjointed, often counterproductive, corporate/insurance centered “medical” environment that we are forced to struggle within. (Note: I did not include “patient centered” in my description of our health care system. Jaded? - ya think?)
Thanks & Keep on keeping’ on..
Christina R. B. Tsuchida
My Doctor recommended avoiding milk products take at the same time as dopamine pills. Something about the 'lactic acid' inhibits the medicine's absorption by the small intestine it seems. Meanwhile general research has shown that yogurt has to be eaten with vegetable fiber in order to be digested! So I found myself dropping yogurt and then even powdered milk (once prized for easing the acidity of coffee). The reduced protein in my diet as a whole has meant freedom to eat whatever else I might want while still losing weight gradually (diagnosed as Parkinson's-disease-ridden in 2011 [at age 63], I am now 73 years old. Our son after Japanese-medium schooling from kindergarten through university graduation [exc. for a non-credit year of college as an exchange student], has taken his doctorate in the US and still is working there. Only recently have the medical staff appreciated my decision to live on here. regardless of many examples of divorce or separation in bicultural marriages.). As beyond retirement-age, we appreciate "shoujin ryouri" or vegetarian simplicity in meals. Yet, a lifetime of eating meat or fish leaves its traces in bodily response: no matter how good the feeling of light, vegetarian fare may be, a day without ANY animal protein may stymie my individual efforts at exercise. [Still not with final answers .....]
Dr.
Hi Jo ~ We can really relate to your difficulties with the medical profession. One of the goals of Dr. C.'s writing is to give readers information about the disease, both scientific and from my personal experiences. We are here for you -- to offer up some information to take back to your providers or just help you get through the PD days.
thanks for reading the columns --
Dr. C.