Discussion
Discussion
FAQs about Rytary
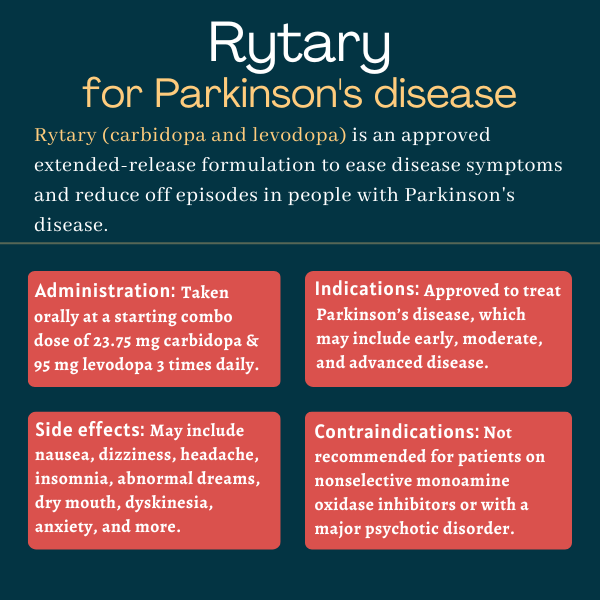
The U.S. Food and Drug Administration approved Rytary in 2015 for the treatment of people with Parkinson’s disease, which may include patients with early, moderate, and advanced disease. The regulatory agency also approved the medication for certain kinds of parkinsonism, or conditions with Parkinson’s-like symptoms.
Based on animal studies, Rytary may cause harm to a developing fetus. However, the therapy has not been well studied in pregnant women so it should be used during pregnancy only if the potential benefits justify the potential risks to the fetus. Patients should always talk to their healthcare providers if they become or intend to become pregnant while on a medication.
Due to reports of people falling asleep during daily activities while on levodopa-based therapies, Rytary’s U.S. label recommends that people initiating therapy should not drive and should avoid other potentially dangerous activities that might result in harm if the patient becomes somnolent.
Based on data from clinical trials, Rytary reaches a peak concentration in the blood about one hour after administration, at which point an easing in Parkinson’s symptoms should already be evident. That effect is then maintained for about 4-5 hours before declining. However, because the initial recommended dose of Rytary may not work for everyone, some patients may require dose adjustments before experiencing the full benefits of the therapy.
Neither hair loss nor weight gain have been reported as side effects of Rytary in clinical trials, but there have been some isolated reports of hair loss in people receiving levodopa-based medications. Weight gain also can occur due to compulsive eating, a potential side effect of the medication. Patients who experience such effects after starting on the Rytary should discuss these issues with their healthcare providers.
Related Articles
 Fact-checked by
Fact-checked by