Discussion
Discussion
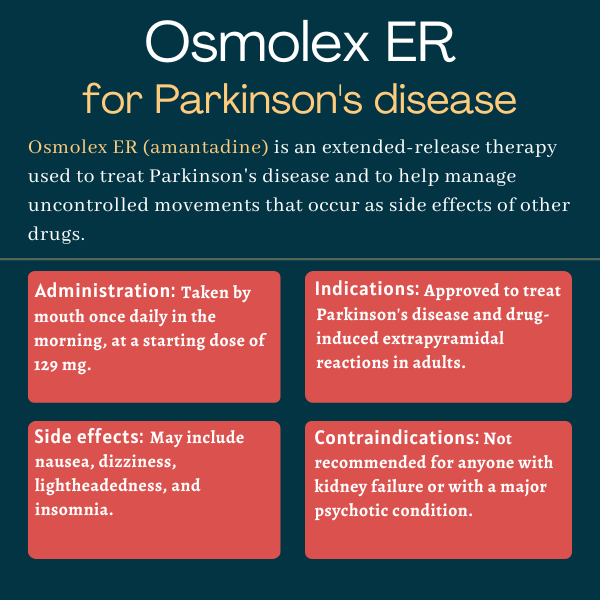
Osmolex ER (amantadine) for Parkinson’s disease
What is Osmolex ER for Parkinson’s disease?
Osmolex ER (amantadine) is an approved, extended-release oral treatment that can be used to ease symptoms of Parkinson’s disease and manage uncontrolled movements that develop as a side effect of other Parkinson’s treatments.
The medication was originally developed by Osmotica Pharmaceutical, but its rights were acquired by Adamas Pharmaceuticals in late 2020 as part of a patent litigation settlement. Adamas was then acquired by Supernus Pharmaceuticals, which currently markets Osmolex ER.
Therapy snapshot
| Brand name: | Osmolex ER |
| Chemical name: | Amantadine |
| Usage: | Used to manage Parkinson’s symptoms and uncontrolled movements that occur as medication side effects |
| Administration: | Extended-release oral tablets |
How does Osmolex ER work?
The symptoms of Parkinson’s arise due to decreased dopamine signaling. Dopamine is a neurotransmitter — a chemical that nerve cells use to communicate with each other — and Parkinson’s is caused by the dysfunction and death of dopamine-making cells in the brain.
The exact mechanism of how Osmolex ER works in Parkinson’s disease is not known, but it’s thought that the therapy increases the release of dopamine by dopamine-making nerve cells while limiting its reabsorption, thus strengthening dopamine signaling.
Osmolex’s delivery method comprises an outer layer of amantadine that dissolves within 30 to 60 minutes after the pill is ingested. Then, the semipermeable tablet shell lets water in without letting amantadine out, which facilitates a steady release of amantadine through a laser-drilled hole in the tablet.
This delivery system allows for once-daily dosing of Osmolex ER.
Who can take Osmolex ER?
Osmolex ER was approved by the U.S. Food and Drug Administration in February 2018. The therapy is indicated to treat Parkinson’s disease itself, and also as a treatment for drug-induced extrapyramidal reactions in adult patients.
Extrapyramidal reactions are a type of uncontrolled movement. Long-term treatment with levodopa, which is widely considered the gold standard Parkinson’s treatment, frequently leads to a type of extrapyramidal reaction called drug-induced dyskinesia.
Who should not take Osmolex ER?
Osmolex ER should not be taken by anyone with kidney failure, when the kidneys can no longer filter waste and excess fluid from the blood to meet the body’s needs.
The therapy also is not generally recommended for patients with a major psychotic condition, as it can increase the risk of a psychosis exacerbation, and patients should not receive any live vaccines while on Osmolex ER.
How is Osmolex ER administered in Parkinson’s?
Osmolex ER is available as round, extended-release tablets that come in two dosage strengths:
- 129 mg, available as white-coated tablets imprinted on one side with a black “VP” over “075”
- 193 mg, available as green-coated tablets imprinted on one side with a black “VP” over “076”
The recommended starting dose of Osmolex ER is 129 mg, taken once daily in the morning. The dosage can then be increased at weekly intervals up to a maximum of 322 mg (taken as one 129 mg and one 193 mg tablet).
The recommended starting and maximum doses are not altered for patients with mild, moderate, or severe kidney impairment, but it’s recommended that the medication be given less frequently, and doses increased over longer intervals, in patients with moderate or severe kidney disease.
Those with renal impairment also should be routinely monitored for changes in kidney function, especially if they have a severe impairment and are taking the maximum 322 mg dose.
Osmolex ER tablets should be swallowed whole and not crushed, chewed, or divided. The medication may be taken without regard to food, but patients taking Osmolex ER should not drink alcohol due to a risk of worsened side effects like dizziness and blood pressure issues.
If a dose is missed, patients should take their usual dose of Osmolex ER on the next day in the morning instead of making up the missed dose.
Because suddenly stopping Osmolex ER can cause problematic reactions, it’s recommended that the dose be gradually decreased over the course of a week or two if the medication needs to be discontinued.
Osmolex ER in clinical trials
The active substance in Osmolex ER, called amantadine, is the same as in Gocovri, another approved Parkinson’s treatment that was developed by Adamas and is now marketed by Supernus.
In clinical trials, Parkinson’s patients given Gocovri had significantly more time spent with well-controlled symptoms and without troublesome uncontrolled movements, known as dyskinesia, compared with patients given a placebo.
The approval of Osmolex ER in the U.S. was based on data from Gocovri trials, as well as bioavailability studies showing that the extended-release formulation delivers a similar amount of amantadine to the body as Gocovri.
In one of these studies, a total of 24 healthy volunteers received a 139 mg dose of Gocovri twice daily for seven days, before or after being given a daily 258 mg dose of Osmolex ER also for seven days. There was a one-week interval between each treatment period.
Data showed that the average daily levels of amantadine in the blood were comparable with twice daily Gocovri and once daily Osmolex ER, supporting the similar bioavailability of the two medications. The extended-release medication reached its peak concentration about 7.5 hours after dosing.
Common side effects of Osmolex
The most common side effects associated with Osmolex ER in clinical trials included:
- nausea
- dizziness or lightheadedness
- insomnia.
Sleepiness
Taking Osmolex ER may cause unusual sleepiness or unintentionally falling asleep. In most cases, treatment should be stopped if this side effect occurs, but if the decision is made to continue Osmolex ER treatment in patients who experience sleepiness, then patients should avoid driving and other activities where falling asleep may be dangerous.
Suicidality and depression
Suicidal thoughts and suicide attempts have been reported in patients treated with amantadine, the active agent in Osmolex ER. The medication may worsen mental health problems in people with a history of psychiatric disorders or substance abuse. Patients should be monitored for depression and suicidal thoughts, and if these occur, the potential risks of continuing the treatment should be carefully considered.
Hallucinations and psychotic behavior
Patients given Osmolex ER, or those who suddenly stop taking the therapy, may experience changes in behavior or psychosis — which can include hallucinations where someone senses something that isn’t there, or delusions which are fixed beliefs that have no basis in observable reality. Patients should be monitored for psychosis throughout treatment with Osmolex ER, especially when starting the therapy or altering the dose.
Osmolex ER should generally not be given to people who already have a major psychotic disorder, as the treatment may worsen the psychosis.
Dizziness and orthostatic hypotension
Osmolex ER may cause dizziness and orthostatic hypotension, a condition where blood pressure suddenly drops when a person stands up from a seated or lying position, which can result in lightheadedness or fainting (syncope). Patients should be monitored for these potential side effects, especially when starting Osmolex ER or increasing the medication’s dose.
Alcohol can worsen these side effects, so it’s recommended that patients should not drink alcohol while taking Osmolex ER.
Withdrawal-emergent fever and confusion
Abruptly stopping treatment with Osmolex ER or other formulations of amantadine can cause a syndrome characterized by high body temperature (hyperpyrexia), rigid muscles, and altered consciousness.
Abruptly stopping amantadine also may worsen Parkinson’s symptoms or cause psychosis and other mental health problems. Because of these risks, the dose of Osmolex ER should be gradually reduced over the course of a week or two if the therapy needs to be discontinued.
Impulsive behaviors
Some people given dopamine-modulating medicines like Osmolex ER experience intense urges to engage in risky behaviors like gambling, spending money, binge eating, or sexual behaviors. These urges may not register as abnormal to the patient themself, so it’s important for clinicians and caregivers to be proactive about monitoring for changes in behavior in individuals taking Osmolex ER.
If abnormal urges develop, treatment with Osmolex ER may be stopped or the dose may be reduced.
Use in pregnancy and breastfeeding
Well-controlled studies assessing the effects of Osmolex ER in people who are pregnant or breastfeeding are still lacking. Data from animal studies have suggested that the therapy’s active ingredient can cause harm to a developing fetus. Also, amantadine has been found in human milk, but it’s not known if it can impact milk production or have a negative impact on the breastfed infant.
In patients on Osmolex ER who are planning to become pregnant or to breastfeed, the potential benefits of Osmolex ER should be carefully weighed against the potential risks.
Parkinson’s News Today is strictly a news and information website about the disease. It does not provide medical advice, diagnosis or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or another qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recent Posts
- Being mad at each other and mad at Parkinson’s disease, too
- Parkinson’s muscle firing patterns different for women than for men
- Breathing CO2 activates brain cleanup signals in new Parkinson’s study
- Guest Voice: DBS surgery transformed my life with early-onset Parkinson’s
- Smartphone app helps Parkinson’s patients map daily symptoms
Related articles
-
 Discussion
Discussion
-
 Fact-checked by
Fact-checked by