Work by 3 biobehavioral scientists aims to support Parkinson’s patients
Teachers College researchers focus efforts on exercise, speech, swallowing
Written by |
Three biobehavioral scientists at Teachers College (TC), Columbia University are working on separate collaborative efforts in exercise, speech, and swallowing among Parkinson’s patients to potentially improve quality of life for the more than 10 million people estimated globally to be living with the progressive neurodegenerative disease.
In honor of this year’s Parkinson’s Disease Awareness Month, observed each April, the New York-based graduate school of education, health, and psychology is highlighting the work of three of its researchers: Gemma Moya-Galé, PhD, Michelle Troche, PhD, and Lori Quinn.
All three are aiming to directly help Parkinson’s patients by incorporating advances in medicine and technology into clinical care, according to a TC university press release highlighting the researchers’ work. The focus of this year’s Awareness Month for many scientists and advocacy groups is on advancing research, and gaining a better understanding of ways to manage Parkinson’s.
“The more I learned about the disease, the more I wanted to help somehow,” said Moya-Galé, whose interest in Parkinson’s research was influenced by an undergraduate professor living with the condition.
“Meeting patients who are advocates… it now has become more personal,” Moya-Galé said.
Scientist seeking to improve services for Spanish-speaking Parkinson’s patients
People with Parkinson’s can have vocal issues and difficulties with speech. Many patients have what’s called hypophonia — an abnormally soft and quiet speaking voice.
An assistant professor and speech-language pathologist, Moya-Galé leads speech therapy classes that are funded by the Parkinson’s Foundation. Thus far, these classes have served more than 60 patients over five years at no charge.
“The group has built an incredible sense of community, especially ever since Covid-19,” said Moya-Galé, noting that bringing patients together is as important as the therapy.
“Something ordinary [like speaking] becomes a hurdle; it makes many people withdraw within themselves, and causes a lot of social withdrawal, loneliness… We already know the effect that those speech problems have on people’s overall quality of life,” she said.
The speech therapy sessions, supported by TC students, include smaller breakout groups to allow more personalized attention to areas such as breathing, voice strengthening, and linguistic skills.
Relatedly, Moya-Galé is seeking to narrow the research and practice gap for Spanish-speaking Parkinson’s patients by studying the intricacies of their speech therapy needs. She hopes to work with such patients directly in a similar therapy group model.
Further, Moya-Galé is collaborating with colleagues on an app that can potentially help Parkinson’s patients practice communicating over background noise. Ambient sounds can be problematic partly due to the disorder’s disruption of volume amplification. The tool is undergoing clinical tests for its effectiveness in speech improvement.
Publishing an exercise guide in collaboration with the MJFF
Efforts by Quinn, a research physical therapist who directs the graduate program in movement sciences and kinesiology and leads the college’s neurorehabilitation research lab, are focused on exercise. A key goal, she notes, is to eliminate treatment barriers in Parkinson’s with the support of community health.
In 2019, Quinn began working with The Michael J. Fox Foundation (MJFF) on Parkinson’s resources, which led to her co-authorship of the MJFF’s 72-page patient guide, titled “Make Your Move: Exercise for Brain Health and Life with Parkinson’s.” That work was done along with TC doctoral candidate Chelsea MacPherson, a physical therapist, and two other Parkinson’s experts.
A large and expanding body of evidence shows that regular physical exercise can stave off Parkinson’s onset, slow the condition’s progression, and mitigate motor symptoms as well as nonmotor problems such as depression.
“People get diagnosed and hear that exercise is important, but a neurologist who is meeting with them for an hour does not have the time to go through what that actually means for someone with Parkinson’s,” Quinn said.
According to Quinn, “people have really struggled, so it was really important for the guide to be evidence-based.”
“We really tried to take the literature and apply it to this book, and that is something that is unique and different,” she said.
We need to include patients with Parkinson’s disease from the very beginning [of research efforts], talking about their lived experience.
Quinn’s work with the MJFF also includes the upcoming book “We Do Research,” which builds upon an illustrated Teachers College resource that addresses care obstacles for Black Parkinson’s patients.
“We need to include patients with Parkinson’s disease from the very beginning, talking about their lived experience and asking them what it is that they need from a book like this,” said Quinn. “This is a very different approach to things, so that has been really great in collaborating with them.”
Parkinson’s patients sought for swallowing trial led by TC researcher
Connecting with patients also is key for Troche, an associate professor of speech and language pathology.
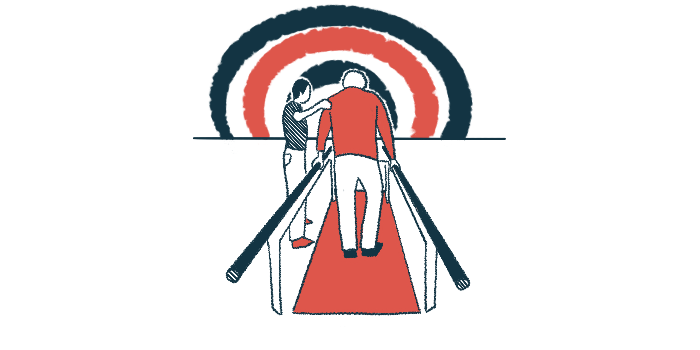
Troche is leading an ongoing, federally funded clinical trial (NCT05700825) that compares in-person and telehealth treatments for cough and swallowing disorders in Parkinson’s. The overarching aim is to expand access to therapies for such conditions.
The study is recruiting participants, ages 50 to 90, at Purdue University, in Indiana, and at Columbia.
Four years ago, an MJFF-funded initial TC study showed that an innovative sensorimotor training program could improve clinical outcomes related to cough and swallowing. Such disorders can lead to serious complications in Parkinson’s.
In 2021, Troche and scientists at TC and Purdue University reported that swallowing disorders may be assessed and treated via telehealth. They subsequently created a tutorial for objective speech measures for those with movement disorders and identified the feasibility of key therapies.
Troche’s upcoming research is expected to reveal further insights into telehealth, which 67% of speech pathologists said in a TC survey they’d like to continue to use in Parkinson’s.