Variability in platelet size may be biomarker for Parkinson’s: Study
Findings suggest potential of repurposing medications to treat brain disorders
Written by |
Researchers have discovered a new genetic link between platelets in the bloodstream and Parkinson’s disease, according to a large-scale genetic study that investigated associations between blood measures and neurological and psychiatric diseases.
Variation in platelet size, called platelet distribution width (PDW), was found to be broader in Parkinson’s patients and may serve as a potential biomarker for diagnosis and predicting outcomes.
“One notable finding was a cause and effect relationship between increased platelet distribution width and risk for Parkinson’s Disease, suggesting that platelet parameters could be potential biomarkers for early detection of Parkinson’s Disease,” Yuanhao Yang, PhD, the study’s first author at the Mater Research Institute and The University of Queensland, in Australia, said in an institute press release.
Findings suggest current therapies may be repurposed to treat Parkinson’s
In addition, altered PDW was associated with changes in the activity of genes that are known targets for approved medications, suggesting some current therapies may be used to treat Parkinson’s.
“We also identified numerous genes shared by specific blood cell measures and brain disorders, some of which are targets of drugs that are approved for other conditions — this represents potential for re-purposing those drugs for common brain disorders,” Yang said.
Jake Gratten, PhD, the study’s senior author and an associate professor at The University of Queensland, added that the findings “provide a foundation for future work to improve prevention and prognosis of common neurological diseases and psychiatric disorders.”
The study, “The shared genetic landscape of blood cell traits and risk of neurological and psychiatric disorders,” was published in the journal Cell Genomics.
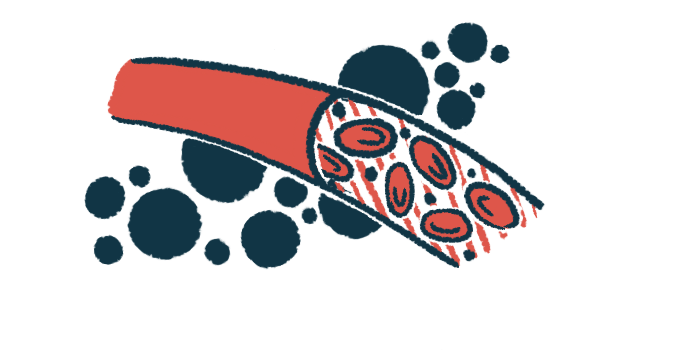
Blood cells include oxygen-carrying red blood cells, immune-mediating white blood cells, and platelets, which are small cell fragments involved in blood clotting.
Variations in the levels and characteristics of blood cells — called blood cell traits (BCTs) — have been linked to neurological disorders, such as Parkinson’s, multiple sclerosis, and stroke, and psychiatric conditions such as major depressive disorder and schizophrenia.
Some disease-related blood cell traits have been shown to have a genetic basis. In addition, the SNCA gene, which encodes for the alpha-synuclein protein and whose mutations are a well-established genetic risk factor of Parkinson’s, also plays a role in the development of red blood cells.
“These results sparked interest in developing blood-based biomarkers for common brain disorders, but it was unclear whether there was a genetic basis to these relationships,” Yang said.
We also identified numerous genes shared by specific blood cell measures and brain disorders, some of which are targets of drugs that are approved for other conditions — this represents potential for re-purposing those drugs for common brain disorders.
Researchers examined large-scale genome-wide association study data sets
To find out, Gratten, Yang, and colleagues in Australia and the U.S. examined data from large-scale genome-wide association study (GWAS) data sets concerning 29 different blood cell traits and 11 common neurological and psychiatric diseases (NPDs).
GWAS involves scanning all genes in an individual’s cells, or the genome, for small genetic alterations, called single nucleotide polymorphisms, or SNPs, found more often in people with a particular disease.
The Parkinson’s GWAS data set included 37,688 cases and 18,618 proxy cases, meaning individuals who do not have Parkinson’s but have a parent, sibling, or child who does, as well as 1.4 million unaffected controls. That previous study looked at potential risk factors across more than seven million SNPs in these participants.
Now, the researchers found significant evidence for a cause-effect relationship between elevated PDW, reflecting greater size variation between platelets, and Parkinson’s. In turn, there was no evidence of a reverse cause-effect association, meaning that higher PDW was not itself caused by Parkinson’s disease.
Increased PDW is a known marker of platelet activation, which has been implicated in neuroinflammation, considered a main contributor to Parkinson’s.
This finding was consistent with recent reports that regular use of anti-inflammatory medications, such as ibuprofen and aspirin that have anti-platelet effects, is protective against Parkinson’s in people carrying mutations in the Parkinson’s-related LRRK2 gene, the team noted.
However, after adjusting for C-reactive protein, a well-established marker for inflammation, the effect of platelet size variation on Parkinson’s remained, “suggesting that the causal effect of PDW on [Parkinson’s disease] may involve platelet functions independent of the inflammatory response,” the researchers wrote.
The team noted that alpha-synuclein, the protein that forms toxic clumps and causes neurodegeneration in Parkinson’s patients, is present in large quantities in platelets, where it regulates essential platelet functions.
“Irrespective of the mechanism, our findings highlight the potential clinical utility of these platelet parameters as potential risk markers and targets for improving prevention and prognosis of PD [Parkinson’s disease],” the researchers wrote.
A total of 60 genes associated with the PDW-Parkinson’s link were identified, some of which represented “interesting candidates for mitigating risk for PD via modulation of platelet activity or function,” the team added.
Notably, 11 of these genes are known targets of currently available medications.
SYK gene activity linked to greater Parkinson’s risk
Greater activity of one of these 11 genes, SYK, which is involved in platelet activation, was found to be significantly associated with increased PDW and higher Parkinson’s risk. This suggests that approved SYK-targeting medications may potentially be repurposed to mitigate Parkinson’s risk.
In addition, elevated activity of the CTNNB1 gene was significantly linked to reduced PDW and risk of Parkinson’s, indicating that medicines that target CTNNB1 may further ameliorate risk.
“We report a broad landscape of genetic overlap between BCTs and common NPDs, finding evidence to suggest that platelet parameters may be useful biomarkers for risk stratification of primary prevention trials of PD,” the researchers wrote.
“Additionally, we identified multiple functional genes and regulatory elements for specific pairs of BCTs and NPDs, some of which are previously unreported, including known drug targets that may present drug re-purposing opportunities for PD,” they concluded.