Stimulating leg nerve shown to reduce tremor in Parkinson’s pilot
Study tested Stimvia's noninvasive URIS device in patients at home
Written by |
Noninvasively stimulating a nerve in the leg using Stimvia‘s URIS device is feasible, safe, and may help reduce motor symptoms and improve quality of life in people with Parkinson’s disease, according to new data from a pilot study.
Indeed, among the small number of patients with tremor in the study, more than two-thirds saw this hallmark Parkinson’s symptom ease after the first six weeks, data showed. By the study’s end, more than 85% of these patients saw their tremors reduced by half.
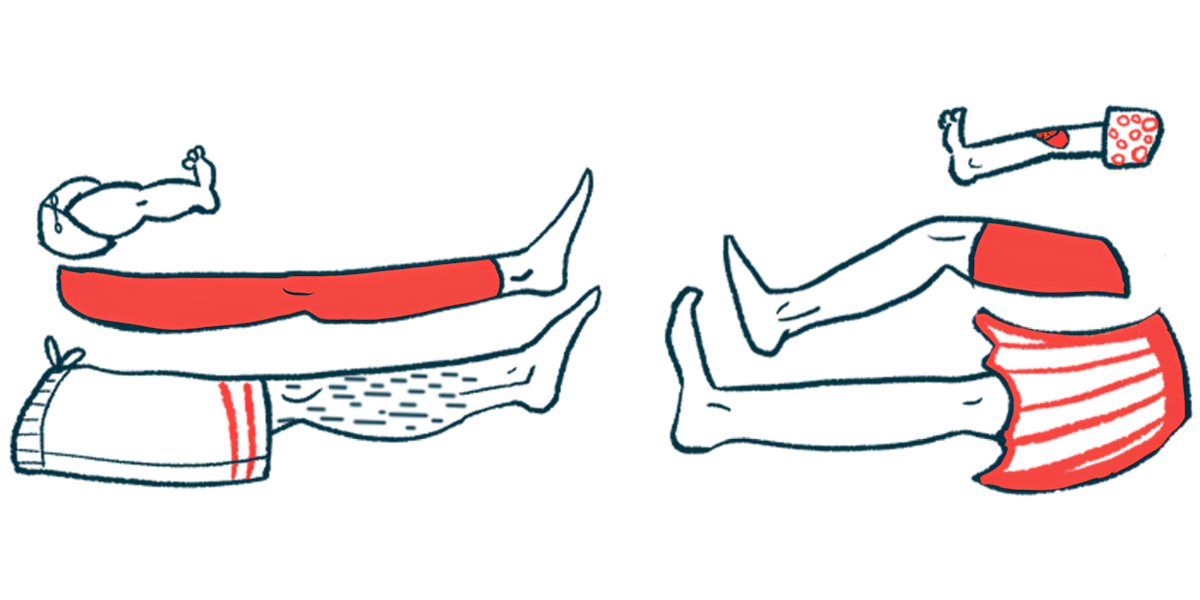
The system, which works by stimulating the peroneal nerve located behind the knee, involves placing self-adhesive electrodes in the leg. It can be used by patients at home — how it was tested in this study — without assistance, per a press release from its developer.
“Patients experienced visible improvements not only in motor symptoms like resting tremor, but more importantly in their everyday comfort and well-being,” said David Skoloudík, PhD, principal investigator of the study and vice dean for science and research at the University of Ostrava in the Czech Republic.
“The changes in quality-of-life questionnaires exceeded the threshold of clinical relevance. And most importantly — there were no severe side effects,” Skoloudík added.
The results were described in a study titled “Home-based peroneal electrical transcutaneous NeuroModulation (peroneal eTNM) in Parkinson’s disease as “add-on” treatment – Results of a pilot study,” which was published in the journal Clinical Parkinsonism & Related Disorders.
Parkinson’s disease is caused by the progressive loss of the nerve cells that produce dopamine, a brain signaling molecule involved in motor control. This leads to a range of symptoms, including motor symptoms like tremor, slowed movements, and muscle rigidity.
URIS, designed for overactive bladder, targets leg nerve located behind knee
Peroneal electrical transcutaneous neuromodulation (eTNM) is an approach in which the peroneal nerve — located behind the knee — is stimulated via electrodes on the skin to control certain functions.
The URIS eTMN neuromodulation system was originally developed to treat overactive bladder, a condition characterized by sudden urges to urinate. But researchers observed that people with Parkinson’s who used the system also experienced an easing of motor symptoms.
That led to this pilot clinical study (NCT06036368), launched to assess whether this system would be a safe, feasible, and effective alternative treatment to manage Parkinson’s motor symptoms, especially for patients experiencing side effects of long-term Parkinson’s treatment.
The trial enrolled 12 adults with Parkinson’s: eight men and four women, with a mean age of 59.5. In addition to their standard Parkinson’s treatment — levodopa, dopamine agonists, or a combination of both — participants used the device for 30 minutes each day at home, for six weeks. This was followed by another six weeks without stimulation to assess if the beneficial effects persisted.
Overall, the treatment was “very well tolerated,” the researchers wrote, noting that “no patient reported pain or any uncomfortable sensations during stimulation.” Further, none of the side effects that occurred during the study were related to treatment, according to the team.
It was also feasible, with patients completing an average of 40 of the 41 total sessions, and no patient requiring assistance to use the device.
By study’s end, over 85% of participants experienced reduction in tremor
A secondary goal of the study, after its safety, was to assess if participants reported any improvements, as assessed with the patient’s global impression of improvement (PGI-I) scale. After the six weeks of treatment, 42% reported an improvement. This percentage increased to 50% after the six weeks without stimulation, suggesting that the benefits were long-lasting, the researchers noted.
Participants also experienced improvements in resting tremor, which tended to increase even after the stimulation sessions had ended. Among the nine patients with tremors, 67% had a reduction in tremors of at least 50% after the initial six weeks. By the end of the study, 89% of patients had achieved such benefits.
We aim to slow [Parkinson’s] progression … and extend patients’ quality years of life — without the need for invasive procedures such as deep brain stimulation. … We’re already seeing that URIS may be a more suitable option in the early stages of Parkinson’s, thanks to its noninvasive nature, ease of home use, and strong safety profile.
There were also improvements in the Parkinson’s Disease Questionnaire, which assesses how often people with Parkinson’s experience difficulties across eight dimensions of daily living. Individual areas of that scale, such as bodily discomfort, emotional, cognition, and stigma also improved with treatment. Finally, patients had better quality of life, especially in domains such as self care and anxiety and depression.
“With the combination of levodopa and noninvasive neuromodulation, we aim to slow the progression of the disease and extend patients’ quality years of life — without the need for invasive procedures such as deep brain stimulation,” said Lukas Doskocil, CEO of Stimvia. Deep brain stimulation is a surgical treatment that involves implanting electrodes into the brain.
“We’re already seeing that URIS may be a more suitable option in the early stages of Parkinson’s, thanks to its noninvasive nature, ease of home use, and strong safety profile,” Doskocil said.
The company says it’s now preparing a larger international clinical trial to confirm the promising results of its pilot study.