Examining skin cells may aid in early Parkinson’s diagnosis
Molecular changes that drive damage to brain cells also occur in fibroblasts
Written by |
Some molecular changes that drive damage to brain cells in Parkinson’s disease take place in skin cells too, a study has found, adding to evidence that examining the skin may support an early diagnosis.
Because skin cells are much easier to collect than brain cells, they also could be used to obtain patient-specific information for personalized medicine, wherein a person’s genetic profile helps determine what treatment to use.
The discovery came about when researchers at the University of Arizona College of Medicine, Tucson started transforming skin cells from adults with Parkinson’s into nerve cells, or neurons, to develop a better model of the disease.
“We wanted to make neurons from skin biopsies [tissue samples],” Lalitha Madhavan, MD, PhD, associate professor of neurology at the College of Medicine, part of University of Arizona Health Sciences, said in a university news release. “However, we noted along the way that the fibroblasts themselves seemed to have signatures that differentiated individuals with Parkinson’s.” Fibroblasts are cells in the underlying layer of the skin, where they help it maintain its scaffold.
Toward an early diagnosis
Those signatures paralleled the molecular changes taking place in dopamine-producing neurons, those gradually lost in Parkinson’s. “It’s exciting that we’ve shown that connection, and that it tells us skin cells could perhaps be used to diagnose the disease early,” Madhavan said.
Using these findings as groundwork, Madhavan has been granted a patent by the U.S. Patent and Trademark Office that covers the use of molecular signatures of dermal (skin-derived) fibroblasts as biomarkers to diagnose and predict the course of Parkinson’s.
The study, “Parallel neurodegenerative phenotypes in sporadic Parkinson’s disease fibroblasts and midbrain dopamine neurons,” was published in Progress in Neurobiology.
Parkinson’s may go undiagnosed for a long time or be misdiagnosed because its symptoms often develop slowly and overlap with those of other diseases. When a diagnosis is made, much neuronal damage may have already occurred.
Other research groups have investigated testing the skin as a way to diagnose Parkinson’s at its early stages by using artificial intelligence to “smell” the skin, swabbing the skin to measure its oily coating, or detecting alpha-synuclein clumps, a disease hallmark.
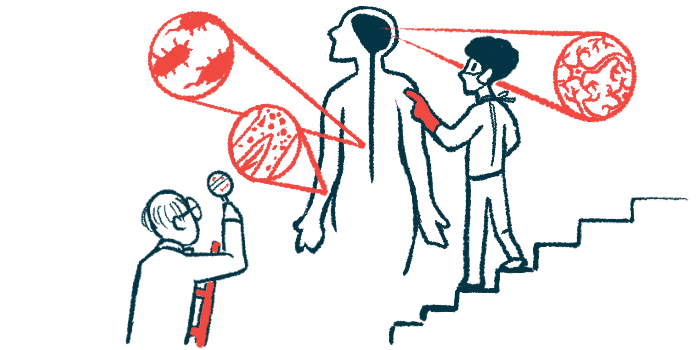
Researchers on Madhavan’s team compared dermal fibroblasts from eight people with idiopathic, late-onset Parkinson’s with those of nine healthy age-matched people. The cells came mainly from the Parkinson’s Progression Markers Initiative repository at Indiana University. Idiopathic means a disease has an unknown cause.
Comparing skin cells
Compared with healthy fibroblasts, those from people with Parkinson’s were smaller and grew faster in number into denser communities of aligned, closely packed cells, with “each cell surrounded by more neighboring cells,” the researchers wrote. They also died faster.
Fibroblasts from people with Parkinson’s also had smaller and misshaped mitochondria with a significantly compromised function. Mitochondria are the cells’ energy generators and their structure and function are affected early in the course of the disease.
Autophagy, a process by which cells break down faulty proteins and debris to recycle for new functions, especially during periods of stress, was higher in the fibroblasts of people with Parkinson’s.
Madhavan’s researchers then used pluripotent stem cell technology, a technique that transforms adult cells into embryo-like cells that can mature into almost any cell type, to remake dermal fibroblasts into dopamine-producing neurons.
The researchers compared cell data from fibroblasts and neurons, correlating it with clinical data from people with Parkinson’s. Like fibroblasts, dopamine-producing neurons from the same people with Parkinson’s were different from those of healthy people in their shape, growth, mitochondria, and autophagy process.
On average, the Parkinson’s group had reduced viability in fibroblasts, but not in neurons. Those with Parkinson’s showed a similar increase in oxidative stress values in both fibroblasts and neurons.
The relative expression of alpha-synuclein was higher in both Parkinson’s neurons and fibroblasts over the healthy counterparts, indicating a similar amount of change in both cell types.
And compared to controls, about twice as many neurons from people with Parkinson’s tested positive for alpha-synuclein and its phosphorylated form, which tends to clump together into toxic aggregates. A larger proportion of neurons were also inactive, or unable to relay messages.
“In essence, we report parallel neurodegenerative phenotypes in sporadic PD [Parkinson’s disease] fibroblasts and matched iPSC-based DA [dopaminergic] neurons, derived from the same patient, which capture several fundamental PD features,” the researchers wrote.
Besides providing a tool to study the mechanisms of Parkinson’s, the cell model “also provides a strong platform for the discovery of biomarkers for the early diagnosis and stratification of [Parkinson’s] patients,” the researchers wrote.
“We’ve been putting Parkinson’s into one big bucket when actually different people express it differently,” Madhavan said. “This system would allow us to carefully classify Parkinson’s and assess treatments more effectively based on such a classification.”