Scientists ID important new mechanism in familial Parkinson’s
Mutation in CHCHD2 gene found to promote alpha-synuclein clumps

The findings of new research identifying the mechanism behind a familial form of Parkinson’s — one caused by a CHCHD2 gene mutation — suggest the potential to delay or perhaps prevent the disease’s development in people with the mutation, according to researchers.
The team of scientists found this CHCHD2 gene mutation leads to an abnormal location of the resulting CHCHD2 protein inside neurons, which in turn promotes the formation of disease-related alpha-synuclein clumps. Behind those toxic clumps is the interaction between the mislocated CHCHD2 protein and the Csnk1e enzyme, which modifies the alpha-synuclein protein in a way that makes it more prone to clumping.
Importantly, blocking Csnk1e and a similar enzyme was found to ease Parkinson’s-associated features both in lab-grown patient-derived neurons and mouse models of CHCHD2-related disease.
“This suggests that it may be possible to delay — or even prevent — Parkinson’s disease development in people with this mutation,” Shigeomi Shimizu, MD, PhD, the study’s senior author, from the Tokyo Medical and Dental University (TMDU), in Japan, said in a press release.
The study, “Involvement of casein kinase 1 epsilon/delta (Csnk1e/d) in the pathogenesis of familial Parkinson’s disease caused by CHCHD2,” was published in the journal EMBO Molecular Medicine.
CHCHD2 gene mutation linked to both familial and sporadic Parkinson’s
Parkinson’s is characterized by the progressive damage and death of neurons producing dopamine — a major brain chemical messenger essential for motor control — in a brain area called the substantia nigra.
“Although most PD [Parkinson’s disease] cases are sporadic, approximately 10% are familial,” the researchers wrote. Familial Parkinson’s refers to cases in which the disease runs in a family and is caused by mutations that are passed down from one generation to the next.
How exactly these mutations cause Parkinson’s is not always clear, but the disease-associated neurodegeneration they trigger is thought to be driven by the accumulation of toxic aggregates, or clumps, of the alpha-synuclein protein.
Now, Shimizu and colleagues in Japan set out to assess the mechanisms behind T61I, a mutation in the CHCHD2 gene that has been linked to a familial form of Parkinson’s in three independent Japanese and Chinese families.
The CHCHD2 gene provides instructions to produce a protein of the same name that usually is localized in mitochondria, which serve as the powerhouses of cells. Mutations in CHCHD2 have been linked to both familial and sporadic Parkinson’s.
T61I-related Parkinson’s is linked to alpha-synuclein buildup and characterized by tremor and slowness of movement.
To better understand how the mutation causes Parkinson’s, the researchers tracked down the CHCHD2 protein inside lab-grown mouse cells that were engineered to make either a working or a T61I-mutated version of the human CHCHD2 protein.
“When we looked at normal CHCHD2 protein in cells, it was located in the mitochondria, which provides energy to the cell,” said Satoru Torii, the study’s first author, also from TMDU.
“But the mutant CHCHD2 was [found] in a very different area — in the cell cytosol,” Torii said. The cytosol is the liquid inside a cell.
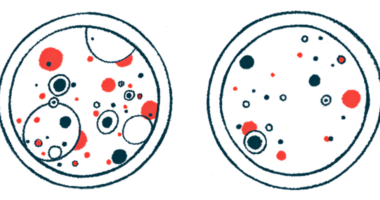
In addition, lab-grown mouse neurons carrying the mutated CHCHD2 showed multiple alpha-synuclein clumps that were co-localized with the mutated protein outside mitochondria. No alpha-synuclein aggregates were seen in neurons making the healthy human CHCHD2 protein.
Neurons producing the T61I-mutated protein also had higher levels of total alpha-synuclein and of phosphorylated alpha-synuclein, a version that is more prone to clumping.
Mutated CHCHD2 protein goes to wrong location inside neurons
Phosphorylation is a process in which a chemical tag, called a phosphoryl group, is added to specific regions in proteins and enzymes, regulating their activity.
Further analyses revealed that the abnormally localized CHCHD2 protein interacted with Csnk1e, an enzyme that works by phosphorylating others. Because Csnk1e shares some functions with Csnk1d, the researchers then looked at both.
They found that Csnk1e/d were co-localized with the mutated CHCHD2 in the cytosol, but not with the healthy version of the protein in mitochondria.
Similar observations were made when analyzing brain slices of a Parkinson’s patient carrying the T61I mutation.
Also, both Csnk1e/d enzymes were found to phosphorylate alpha-synuclein in lab-grown mouse neurons. The enzymes also caused the same type of modification to neurofilament light chain (NfL), a biomarker of nerve cell damage.
Adding PF-670462, a known suppressor of Csnk1e/d, to the mouse neurons producing the mutated CHCHD2 prevented alpha-synuclein from becoming phosphorylated and building up into clumps. NfL phosphorylation also was reduced, but the localization of the mutated CHCHD2 was unchanged.
These findings highlighted that when mutated CHCHD2 was abnormally localized in the cytosol, “it recruited another protein known as casein kinase 1 epsilon/delta (Csnk1e/d) and led to the aggregation of phosphorylated alpha-synuclein and neurofilaments,” Torii said.
The most exciting finding for us was that, when we [suppressed] … Csnk1e/d, we saw motor improvements and fewer Parkinson’s disease-related symptoms in the Parkinson’s disease model mice, as well as less [disease features] in cells grown from a patient with a CHCHD2 gene mutation.
Similar findings were obtained in lab-grown dopamine-producing neurons derived from a patient carrying that mutation and two mouse models with the T61I mutation.
The researchers found that mice engineered to make the mutated CHCHD2 protein showed poorer motor performance and a reduction in dopamine-producing neurons when compared with healthy mice.
These mice also showed alpha-synuclein clumps in dopamine-producing neurons — and “some of them were shrinking and dying,” the researchers wrote.
Injecting PF-670462 directly into the mice’s brain eased motor symptoms and prevented the death of dopamine-producing neurons. However, it did not have any effect on the location of mutated CHCHD2 in cells.
“The most exciting finding for us was that, when we [suppressed] … Csnk1e/d, we saw motor improvements and fewer Parkinson’s disease-related symptoms in the Parkinson’s disease model mice, as well as less [disease features] in cells grown from a patient with a CHCHD2 gene mutation,” Shimizu said.
“These data provide a foundation to test whether Csnk1e/d could be a pharmacological biomarker of other PD types, and whether its inhibitor could be a candidate for PD therapy,” the researchers concluded.