Noninvasive deep brain stimulation shows promise for Parkinson’s
URIS device was tested on 12 women in a pilot clinical trial
Written by |
Early preliminary data from a pilot study by Stimvia shows a noninvasive neuromodulation device known as URIS eased symptoms among participants in a pilot clinical trial and may serve as an add-on treatment for Parkinson’s disease. The device’s developer plans to release the complete data in the coming months.
“We are pleased to share preliminary findings indicating promising results. Patients have reported improvements in both the number of Parkinson’s disease symptoms and their overall quality of life. Furthermore, we have observed a notable reduction in resting tremor. While the precise data are still under rigorous evaluation, we remain cautiously optimistic about the potential implications of these outcomes,” said David Skoloudik, MD, PhD, the study’s lead investigator and vice dean for Science and Research at the Medical Faculty of Ostrava University, Czech Republic, in a company press release.
Parkinson’s is caused by the loss of nerve cells that produce dopamine, a major brain chemical messenger that helps control movement. Their loss leads to disease symptoms , including tremor and slowed movements.
Deep brain stimulation (DBS) has been used to treat Parkinson’s motor symptoms and those with a poor response to other therapies. With DBS, electrodes are surgically placed that deliver electrical stimulation to specific areas of the brain. The electrical current, which is generated by a battery-powered neurostimulator implanted under the skin, blocks the signals that underlie Parkinson’s motor symptoms, such as tremors.
Testing URIS for Parkinson’s
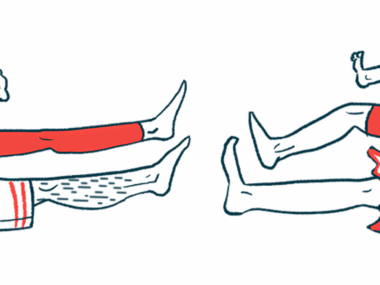
Stimvia’s URIS device uses electrodes placed near the peroneal nerve in the lower leg to modulate electrical activity that stimulates specific nerve pathways in the brain.
It functions as a noninvasive alternative for DBS to modulate the activity of specific brain nerve pathways. A built-in monitoring system lets doctors monitor the brain’s response to the stimuli, adjusting the neurostimulation as needed.
Twelve women with Parkinson’s disease and essential tremor in the pilot clinical trial (NCT06036368) used the URIS device daily for 30 minutes over six weeks. They were all followed for another six weeks without any stimulation to monitor the treatment’s persistence..
The main goal was to assess the safety and tolerability of the URIS device. Its effectiveness was assessed using the clinician-assessed Patient Global Impression of Improvement scale. Other Parkinson’s efficacy exploratory parameters included changes in overall disease and motor symptoms, and quality of life.
“Since the URIS technology demonstrated a positive impact in treating Parkinson’s disease, Stimvia plans substantial investment in further clinical trials to validate the method’s efficacy and safety. We believe our technology can introduce new, additive treatment modalities for millions of patients who currently have no other options, potentially offering a positive disease-modifying impact on those with Parkinson’s disease,” said Lukas Doskocil, Stimvia’s CEO.
The URIS nerve stimulation device was also tested in a clinical trial (NCT05211193) involving people with overactive bladder. The results showed it reduced the urge to urinate by 80%. The study also observed significant activation of brain regions involved in perceiving bladder fullness.