Parkinson’s May Have 2 Distinct Subtypes, Researchers Suggest
Parkinson’s disease can be characterized as two different subtypes: one that starts in the brain and one that starts in the gut, a recent study suggests.
This knowledge may open the door for the development of more personalized therapies, which could be based on the particular disease pattern of an individual with Parkinson’s.
The study, “Brain-first versus body-first Parkinson’s disease: a multimodal imaging case-control study,” was published in the journal Brain.
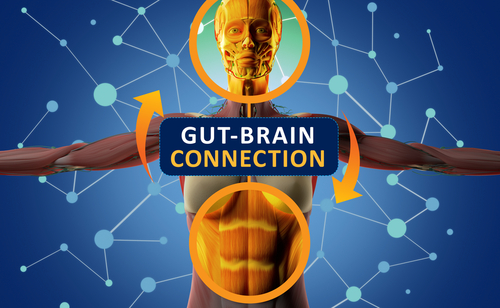
Although Parkinson’s is often considered a neurological disorder that mainly affects the brain, other systems and organs in the body, particularly in the gastrointestinal tract, are thought to play an important role in the disease.
A hallmark of Parkinson’s disease is the buildup of alpha-synuclein protein in the nervous system. Alpha-synuclein aggregates are found mainly in dopamine-producing nerve cells, or neurons, in the brain, where they appear to be involved in neuronal communication. However, it has not been entirely clear up to this point where the initial alpha-synuclein toxic aggregates originate.
Researchers at Aarhus University and Aarhus University Hospital in Denmark hypothesized that Parkinson’s disease is actually divided into two subtypes, according to the initial site of alpha-synuclein aggregation.
In the brain-first subtype, alpha-synuclein would build up in the brain and spread to the peripheral autonomic nervous system — which controls involuntary bodily actions such as blood pressure or digestion.
In the body-first subtype, alpha-synuclein aggregates would originate in the enteric nervous system — the nervous system of the gut — and then spread to the brain, where they would gradually damage and destroy brain cells.
To test their hypothesis, the researchers quantified neuronal dysfunction using advanced scanning techniques, including positron emission tomography and MRI, in 37 individuals with clinically probable Parkinson’s disease (age range 50–85 years), of whom 13 had premotor sleep behavior disorder (RBD), with a median symptom duration of 12.8 years. RBD is a condition in which people act out their dreams, resulting in mild to violent limb movements and talking.
Published data from 22 patients with isolated RBD (iRBD) were used for comparison, as this specific population is at an increased risk of developing the disease. The study was conducted between August 2018 and January 2020.
Imaging parameters were analyzed, using statistical methods, in these three distinct groups and a group of healthy people who were used as a controls for comparison purposes, but not included in the analysis.
Other assessments besides imaging included motor and non-motor symptoms, constipation, cognitive status, sleepiness, depression, orthostatic hypotension (drop in blood pressure upon standing up), and sense of smell.
The researchers found there was a comparable number of motor and non-motor symptoms between patients with and without RBD and a similar dopamine deficit, but they found strikingly different imaging profiles between these two groups of patients.
The combined iRBD and RBD patient data were compatible with a body-first trajectory, characterized by damage to the nervous system of the intestines and heart before the damage in the brain’s dopamine system was visible. These individuals had abnormally enlarged colon (large intestine) volumes and intestinal transit times, although the iRBD group was less affected.
In contrast, the scans from patients without RBD were compatible with a brain-first trajectory: with initial brain damage prior to damage in the intestines and heart.
These data support the hypothesis of the existence of two subtypes of Parkinson’s disease, and show that the presence of RBD before motor symptoms are visible is a highly predictive marker of the body-first subtype.
“It has long since been demonstrated that Parkinson’s patients have a different microbiome in the intestines than healthy people, without us truly understanding the significance of this,” Per Borghammer, MD, PhD, a professor at Aarhus University, said in a press release. “Now that we’re able to identify the two types of Parkinson’s disease, we can examine the risk factors and possible genetic factors that may be different for the two types. The next step is to examine whether, for example, body-first Parkinson’s disease can be treated by treating the intestines with feces transplantation or in other ways that affect the microbiome.”
The researchers believe that this knowledge can offer hope “for better and more targeted treatment of people who are affected by Parkinson’s disease in the future.”






