Parkinson’s cell therapy bemdaneprocel shortens off time
Trial data show treatment also increases time with controlled symptoms
Written by |

Adults with Parkinson’s disease treated with the cell therapy bemdaneprocel spent less time in off periods, when symptoms were not adequately controlled despite medication use. That’s according to final published data from the exPDite Phase 1 trial (NCT04802733), which also showed that the cell therapy boosted the time with well-controlled symptoms.
Bluerock Therapeutics expects to launch a Phase 3 clinical trial, exPDite-2, in the first half of this year to confirm the findings.
“The results of this early phase clinical trial demonstrate the promise of regenerative medicine and should provide hope for Parkinson’s disease patients and their families,” Claire Henchcliffe, MD, one of the study’s principal investigators and chair of neurology at the University of California, Irvine, said in a company press release.
Final trial data were reported in the study, “Phase I trial of hES cell-derived dopaminergic neurons for Parkinson’s disease,” published in Nature.
Parkinson’s is caused when the cells in the brain responsible for making the chemical messenger dopamine die over time. Because dopamine helps control movement, its gradual loss gives rise to Parkinson’s symptoms.
Parkinson’s cell therapy aims to ‘rebuild’ brain networks
Levodopa and its derivatives are the standard treatment for Parkinson’s, providing the brain with materials to make more dopamine. While these therapies can be effective for managing symptoms, most patients will experience off periods.
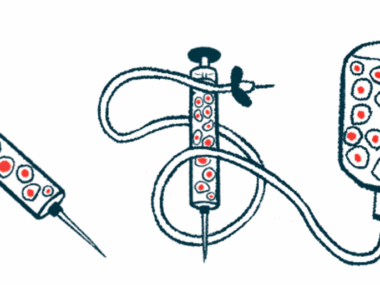
Bemdaneprocel (formerly BRT-DA01) involves surgically transplanting dopamine-producing nerve cells, derived from human embryonic stem cells, into the brain. The goal is for the transplanted cells to grow more nerve cells, produce more dopamine, and ease symptoms.
“The concept of ‘rebuilding’ brain networks that have been lost to disease is compelling,” Henchcliffe said.
The exPDite trial evaluated bemdaneprocel in 12 adults with Parkinson’s who were experiencing off episodes despite levodopa treatment. Five participants were randomly assigned to a low dose (0.9 million cells) of bemdaneprocel, while seven received a high dose (2.7 million cells), into the putamen, a region of the brain involved in movement. They then received one year of immunosuppression to prevent the immune system from attacking the transplanted cells.
As previously reported, no side effects related to the cell therapy were observed two years after the surgical procedure, one year after stopping immunosuppression.
The newly published data report the final outcomes collected 18 months (1.5 years) after treatment compared with baseline (before treatment).
While patients were off medication, high-dose bemdaneprocel lessened motor symptoms, as indicated by a mean drop of 23.0 points in part III of the MDS-Unified Parkinson’s Disease Rating Scale (MDS-UPDRS). The low-dose group also saw a lessening in motor symptoms, with an 8.6-point reduction. The mean time in a good on state, when patients experience satisfactory motor symptom control with levodopa, increased by 0.2 hours in the low-dose group and 2.7 hours in the high-dose group.
While on medication, motor symptoms lessened, with a mean decrease of 8.4 points in MDS-UPDRS scores at the high dose and a 7.6-point reduction at the low dose. The mean off times were shortened by 0.8 hours in the low-dose group and 2.7 hours in the high-dose group.
The ability to perform daily tasks improved in patients who received the high dose of bemdaneprocel, as indicated by a mean decrease of 2.7 points using the MDS-UPDRS part II scale. Conversely, the low-dose group declined in daily task performance, with a 2.4-point increase.
A high dose of the cell therapy also boosted quality of life, as marked by a mean 4.2-point decrease on the Parkinson’s Disease Questionnaire-39 (PDQ-39). In contrast, the quality of life worsened in the low-dose group, with a mean increase of 0.4 in PDQ-39 scores.
No changes were noted in the use of antiparkinsonian medications; the on time periods with troublesome levodopa-induced dyskinesia, or uncontrolled movements; or the severity and impact of dyskinesia, as measured using the Unified Dyskinesia Rating Scale (UDysRS). Nonmotor symptoms showed a trend towards stability at the high dose.
To assess the survival of transplanted cells, patients underwent 18F-DOPA PET imaging studies, which measured the uptake of radioactive L-DOPA, a precursor to dopamine, into dopamine-producing nerve cells. At 18 months after the procedure, and six months after discontinuation of immunosuppression, 18F-DOPA uptake increased, indicating successful graft survival.
Patients who completed the exPDite trial can enroll in its extension study (NCT05897957) to continue monitoring safety and clinical outcomes for up to five years.
“Cell therapy is a potential new treatment option for individuals with Parkinson’s disease and our team is immensely proud of having bemdaneprocel’s 18-month Phase 1 data published in such a prestigious journal as Nature,” said Amit Rakhit, MD, chief medical officer at Bluerock. “Our efforts are now focused on maintaining our forward momentum to initiate and enroll the Phase 3 trial as we advance bemdaneprocel’s development to this exciting next stage.”