MRI-AI model may help distinguish Parkinson’s, atypical parkinsonism
Neuropacs says its technology showed 96% accuracy in imaging study
Written by |
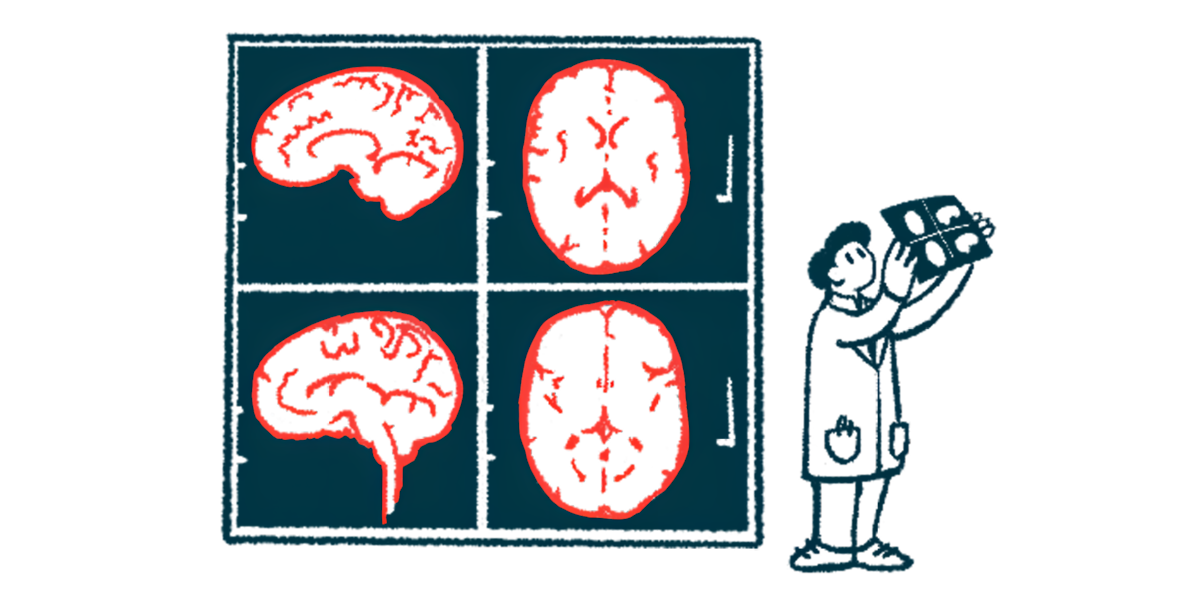
Neuropacs‘ MRI-based artificial intelligence (AI) technology demonstrated 96% accuracy in distinguishing Parkinson’s disease from atypical parkinsonism — including multiple system atrophy, known as MSA, and progressive supranuclear palsy, called PSP — the company announced, detailing the results of a federally funded U.S. study.
Moreover, the system achieved 98% accuracy in differentiating between MSA and PSP, with diagnoses confirmed in about 94% of post-mortem brain analyses, according to a Neuropacs press release.
“This is an important milestone for the parkinsonism community, including clinical providers and, most importantly, patients,” said David Vaillancourt, PhD, Neuropacs’ cofounder and chief scientific officer, a professor at the University of Florida, and the principal investigator of the study. The work was funded by a grant from the National Institute of Neurological Disorders and Stroke, part of the National Institutes of Health.
“We anticipate that the Neuropacs AI technology will revolutionize the current standard of care for diagnosing parkinsonism and will have far-reaching impacts on clinical care and clinical trial testing of new therapeutics,” Vaillancourt said.
The study, “Automated Imaging Differentiation for Parkinsonism,” was published in the journal JAMA Neurology.
Symptoms of atypical parkinsonism often similar to Parkinson’s
Atypical parkinsonism refers to conditions that cause symptoms closely resembling those of Parkinson’s — which can make a diagnosis challenging even for the most experienced clinician. It is estimated that as many as 45% of patients initially diagnosed with Parkinson’s are later found to have another type of parkinsonism.
As such, there is a need to develop clinical biomarkers that can help guide clinicians in reaching a more specific diagnosis.
In this study, scientists assessed Neuropacs’ AI technology in 249 patients at 21 Parkinson Study Group centers — 19 in the U.S. and two in Canada. The patients had a mean age of 67.8, and were mainly men (62%). Based on a consensus clinical diagnosis from three independent neurologists, 99 patients in the study were diagnosed with Parkinson’s, 97 with PSP, and 53 with MSA.
Diffusion magnetic resonance imaging, which captures images based on the movement of water molecules within tissues, was performed on patients and analyzed using Neuropacs’ AI software to predict each individual’s diagnosis.
More than three-quarters of the patients (78%) were placed in a training set to help the AI algorithm learn to differentiate between these types of conditions. The remaining 22% were assigned to a testing set to evaluate the model’s accuracy in diagnosing the conditions.
Patient autopsy data confirmed AI model diagnosis in 94% of cases
According to the data, the model demonstrated a strong accuracy in distinguishing between different conditions, achieving accuracy of 96% in differentiating Parkinson’s from atypical parkinsonism. When distinguishing MSA from PSP, accuracy reached 98%. Similarly, it was 98% accurate in differentiating Parkinson’s from MSA and Parkinson’s from PSP, per the study.
The researchers further confirmed the model predictions by analyzing brain tissue obtained from 49 patient autopsies, with about three years separating the last imaging scan and the individual’s death.
The diagnosis predicted by the AI model was confirmed in 46 of these patients (94%), including in all participants with Parkinson’s or MSA (five patients each), and 36 of 39 individuals with PSP.
This represented a 12.3% gain in obtaining a correct diagnosis compared with a diagnosis based on clinical criteria, the researchers noted. Using clinical criteria, 82% of the patients were correctly diagnosed — four of five with Parkinson’s, three of five with MSA, and 33 of the 39 with PSP, according to the team.
The age of using data-driven tools like AI to diagnose Parkinson’s and other neurological conditions has arrived. … As clinicians, we must embrace these technologies and start considering how we can best integrate them into routine workflows for neurological care.
“The findings highlight the transformative potential of this diagnostic software in clinical practice,” said Michael Okun, MD, codirector of the Norman Fixel Institute at the University of Florida, one of the sites that contributed to the study. Okun also serves as medical advisor for the Parkinson’s Foundation, and is a member of Neuropacs’ clinical advisory board.
“The age of using data-driven tools like AI to diagnose Parkinson’s and other neurological conditions has arrived,” Okun said. “As clinicians, we must embrace these technologies and start considering how we can best integrate them into routine workflows for neurological care.”
Kristophe Diaz, PhD, executive director and chief science officer of CurePSP, a New York-based nonprofit, noted that “proper diagnosis of PSP remains a critical need,” to ensure patients receive the correct treatment.
“The results of this study are exciting progress [toward] a noninvasive and clinically scalable solution to help improve diagnosis,” Diaz said.