Impaired Mitochondrial Recycling Drives Neuron Death in Parkinson’s, Study Indicates
Impaired recycling of mitochondria — the powerhouses of the cell — may drive the loss of the neurons at the heart of Parkinson’s disease, according to a new study.
Boosting the cell’s ability to remove old mitochondria and produce new ones then may prove an effective way to prevent the loss of those neurons.
The study, “Defects in Mitochondrial Biogenesis Drive Mitochondrial Alterations in PARKIN-Deficient Human Dopamine Neurons,” was published in the journal Stem Cell Reports.
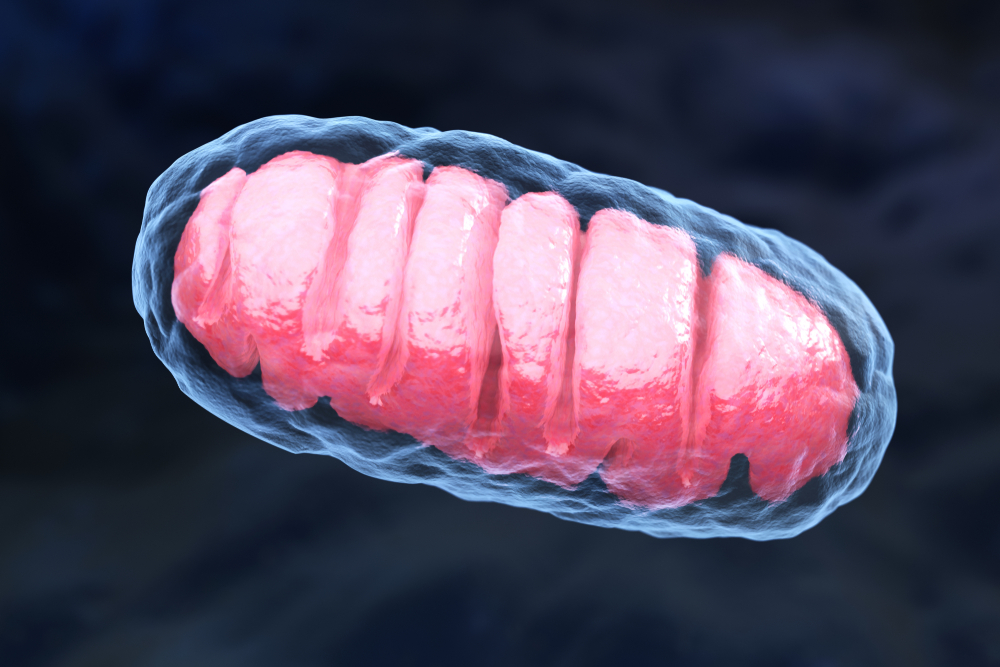
Mitochondria are membrane-enclosed structures within cells that produce energy; they suffer damage over the course of Parkinson’s disease.
Research has shown that mutations in the PRKN gene are linked both to a hereditary form of Parkinson’s disease and to clearing away damaged mitochondria — a process called mitophagy.
Other studies have shown that the accumulation of a protein called Parkin Interacting Substrate (PARIS) also drives the loss of dopamine-producing (dopaminergic) neurons in animals lacking the PARKIN protein that mimic Parkinson’s disease.
Dopamine is an important molecule used in passing information between neurons, coordinating movement, and regulating moods. The loss of dopaminergic neurons is a hallmark of Parkinson’s progression.
These past observations led researchers at Johns Hopkins University Medical School in Maryland to explore the role that defective mitochondrial recycling plays in dopaminergic neuron loss.
The researchers examined dopaminergic neurons that had mutations in the PRKN gene that they either derived from Parkinson’s patients or grew from embryonic stem cells.
These cells all showed declines in mitochondrial energy production, also called mitochondrial respiration, and an inability to clear away old and damaged mitochondria.
The investigators also noticed that cells lacking PARKIN protein had higher amounts of active PARIS, which is known to repress the activity of PGC-1alpha, a gene that regulates mitochondrial production and helps to manage the cell’s oxidative stress — an imbalance between the production of free radicals and the ability of cells to detoxify them, leading to cellular damage.
Cells lacking PARKIN and with higher active PARIS produced fewer mitochondria.
The researchers then examined the role of mitochondrial recycling in the survival of dopaminergic neurons by restoring healthy copies of the PRKN gene to cells with the lost or damaged version and by deleting PARIS from cells that also lacked PARKIN protein.
The two procedures produced different, but complementary, results.
Restoring healthy PRKN rescued the defects in mitophagy. Reducing PARIS levels restored the cells’ ability to produce new mitochondria, thereby also restoring mitochondrial respiration to healthy levels.
The results imply that mitochondrial deficits seen in dopaminergic neurons in Parkinson’s disease occur because the loss of PARKIN causes an increase in the amount of PARIS in the cell, which disrupts mitochondrial recycling.
Although these results do not preclude the possibility that other factors also influence that process, they do highlight the role that mitochondrial recycling plays in the survival of dopaminergic neurons.
They also point toward PARIS as a new potential therapeutic target to prevent the loss of dopaminergic neurons in Parkinson’s.
“Targeting PARIS with drugs to lower its protein levels may provide a new way to treat Parkinson’s disease,” Ted Dawson, MD, PhD, professor of neurology and the study’s senior author, said in a press release.






