Helping Nerve Cells Clear Damaged Mitochondria May Treat Parkinson’s, Study Finds
Written by |
Parkin protein deficiency — which is associated with early onset Parkinson’s disease — is only detrimental when dopamine-producing neurons undergo a metabolic switch as they mature, a new study reported.
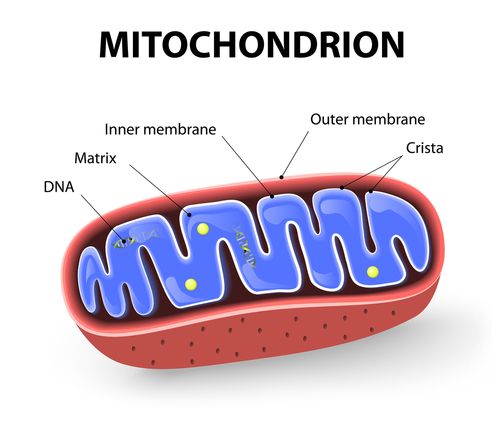
Under such conditions, nerve cells lacking in parkin cannot effectively recycle damaged mitochondria (the cells’ powerhouses, or energy sources), significantly increasing the levels of mitochondrial reactive oxygen species and promoting nerve cell death.
Of note, reactive oxygen species (ROS) are natural byproducts of chemical processes which, when not cleared properly, result in oxidative stress, or the imbalance between ROS production and clearance, which can damage and kill cells.
“Parkin is involved in recycling dysfunctional mitochondria in the cell, so if parkin doesn’t work properly, dysfunctional mitochondria are not efficiently cleared,” Heather Mortiboys, PhD, the study’s senior author at the University of Sheffield’s Institute of Translational Neuroscience (SITraN), said in a university press release.
“This study has shown this is only the case if the cells rely on the mitochondria for their energy supply,” she added, noting that “in cells which can use other energy generating pathways, dysfunctional mitochondria are recycled via alternative pathways.”
Notably, ROS-modulating compounds already being clinically tested in other disorders were found to result in mild improvements in parkin-deficient nerve cells by boosting mitochondrial recycling (a process known as mitophagy).
“This has implications for how easily different pathways can generate the energy the cell needs, and importantly the recycling of defective mitochondria,” said Mortiboys, who is also a senior research fellow for Parkinson’s UK, which funded the research.
These findings may help in identifying new ways of targeting mitochondria, and alternative pathways of mitophagy, to treat Parkinson’s.
The study, “Oxidative switch drives mitophagy defects in dopaminergic parkin mutant patient neurons,” was published in the journal Scientific Reports.
Since nerve cells require large amounts of energy, defects in mitochondria have been linked to several neurodegenerative diseases, including Parkinson’s. However, the exact mechanisms by which dysfunctional or damaged mitochondria contribute to neuronal death remain largely unclear.
“There is debate as to whether the [damaging] component of [mitochondrial abnormalities] is actually loss of energy or increased ROS production,” the researchers wrote.
Researchers at SITraN, along with colleagues in the Netherlands and Australia, found evidence likely supporting the latter, at least in people with Parkinson’s disease caused by PRKN mutations.
Previous studies showed that mutations in the PRKN gene, which provides instructions to produce the parkin protein (involved in mitophagy), are the most common cause of early onset Parkinson’s, generally defined as disease diagnosed in people before age 50.
The team used dopamine-producing neurons (those progressively lost in this disorder) generated from induced neural progenitor cells (iNPCs) derived from four Parkinson’s patients carrying PRKN mutations, and four age- and sex-matched healthy individuals.
iNPCs are derived from fully matured cells that are reprogrammed back to a progenitor state, so they can give rise to all nerve cell types that populate the brain and spinal cord. They also can be genetically modified to carry known disease-causing mutations, or derived directly from patients to be used as cellular models that mimic a disease’s genetic and clinical diversity.
The researchers analyzed cell death and shape, as well as mitochondrial shape, function, recycling, and ROS levels while iNPCs matured into dopamine-producing neurons.
Dopaminergic neurons derived from patients with PRKN mutations were found to have more structural abnormalities and higher death rates at the final maturation stage than those derived from healthy donors.
At this maturation stage, patients’ dopaminergic neurons also showed pronounced changes in mitochondrial shape and function, significantly higher mitochondrial ROS levels, and a severe lack of mitophagy, again compared with these same-stage cells from healthy donors.
Notably, these changes in PRKN-mutated nerve cells coincided with a natural metabolic switch from glycolysis — the energy-producing metabolic reaction based on the breakdown of sugar (glucose) inside cells — to oxidative phosphorylation (an energy-producing reaction that takes place in mitochondria) in maturating nerve cells.
“Our study has found, for the first time, that mitochondrial defects are only revealed when neurons mature and are reliant on their mitochondria to power them,” Mortiboys said.
These findings suggested that upon the metabolic switch, PRKN-mutated dopamine-producing neurons “have impaired basal mitophagy and are unable to mount a response to global mitochondrial dysfunction,” the researchers wrote.
Treatment with ROS-modulating therapies (KH176 and its active form KH176m) — currently in clinical trials for people with mitochondrial disorders — partly reversed the neuronal deficits seen in patient-derived dopamine-producing neurons.
Notably, while such treatments did not change mitochondrial function, they significantly lowered mitochondrial ROS levels and increased mitophagy rates. This suggested that excessive ROS levels, rather than loss of energy, may be behind the damaging effects associated with mitochondrial damage, at least in some Parkinson’s patients.
“Our data suggest a reversal of the energy deficit may not be required to have beneficial neuronal effects; however further work needs to be done to fully investigate this, particularly over a longer term treatment,” the researchers wrote.
Future studies are needed to confirm these findings, and to better understand the implications of this metabolic switch and determine which mitophagy pathway (one not dependent on parkin) is used in PRKN-mutated neurons.
“We’re delighted to be supporting this promising, groundbreaking research,” Claire Bale, head of research at Parkinson’s UK, said in the release, noting that “this study adds a new layer to our understanding of what goes wrong inside brain cells in Parkinson’s and could lay the foundations for developing new treatments.”
“We’re working with Dr Mortiboys through our pioneering Virtual Biotech programme to create new treatments targeting mitochondria which could slow or stop Parkinson’s — something no currently known treatment can do.”


