GCase Mutations Prevent Clearing of Toxic Clumps, Treatment Possible
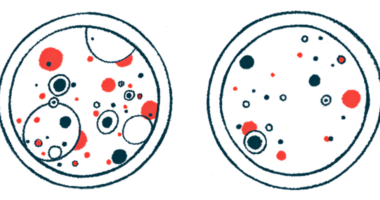
Mutations in the enzyme glucocerebrosidase (GCase) prevent it from entering the lysosome — a cell’s recycling center — where it clears away unwanted materials such as alpha-synuclein toxic clumps that cause Parkinson’s disease and ultimately kill nerve cells, a recent study found.
These encouraging findings may help to validate efforts to repurpose medications approved for other disorders to treat Parkinson’s, Cure Parkinson’s reported on a webpage. Treatment repurposing is a goal of the U.K. nonprofit’s International Linked Clinical Trials program, and a Phase 2 trial found that an existing medication called ambroxol might protect neurons against alpha-synuclein clumps via its effects on GCase activity.
Ambroxol, a type of respiratory medicine, has been shown to increase GCase activity and improve how lysosomes work. It’s also been shown to prevent the death of cells with mutations in GBA — the gene providing the instructions to make GCase.
The study, “Mutant glucocerebrosidase impairs α-synuclein degradation by blockade of chaperone-mediated autophagy,” was published in Science Advances by an international team of researchers led by David Sulzer, PhD.
Sulzer is a professor of psychiatry, neurology, and pharmacology at Columbia University, and he sits on the International Linked Clinical Trials committee.
The lysosome contains enzymes that break down materials that are no longer needed into building blocks that can be reused and built upon by cells.
Alpha-synuclein can be broken down within the lysosome via a process called chaperone-mediated autophagy. For this to occur, the alpha-synuclein protein must be recognized by a special type of molecule called a chaperone. Among other roles, a chaperone prevents proteins from clumping together and helps deliver them to the lysosome for disposal. (Autophagy is a natural process used by cells to degrade damaged or unwanted components.)
GCase is also transported to the lysosome, where it breaks down two types of fatty molecules — glucosylceramide and glucosylsphingomyelin.
Mutations in this enzyme are linked to an increased risk of developing Parkinson’s, and up to 20% of Parkinson’s patients have one copy of a mutated GBA gene.
Researchers found that GCase mutations make the enzyme stick with a chaperone to the outside of the lysosome, blocking other proteins from getting inside and being broken down via autophagy.
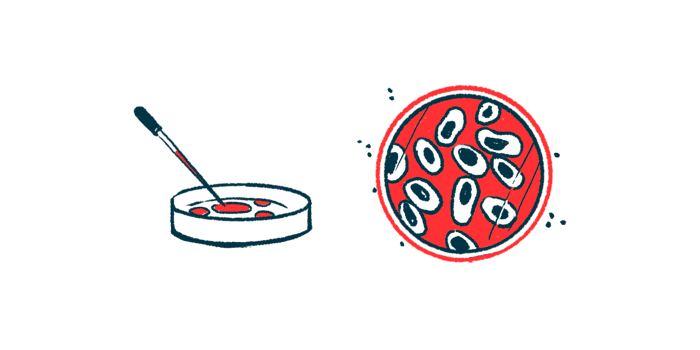
The researchers first tracked down the enzyme inside cells with either a healthy (wild-type) or a mutated version of GCase. They found that the wild-type version was present at higher levels within lysosomes than the mutated version.
They next confirmed this finding in the brains of mice and post-mortem brain tissue from idiopathic (of unknown cause) Parkinson’s patients and people without this disease as a control group. Samples came from 12 patients without GBA mutations, 13 patients with one copy (heterozygous) of a mutated GBA gene, and seven age-matched controls.
“We found … that only subjects heterozygous for [mutated] GCase exhibited GCase on the [outside] of lysosomes, where we also detected high levels of established CMA [chaperone-mediated autophagy] substrates, including [alpha]-synuclein,” the researchers wrote.
The scientists then turned their attention to the specific portion of GCase (called a motif) needed for the enzyme to enter the lysosome. They already knew that a special motif of five protein building blocks, known as a pentapeptide motif, is needed for chaperone recognition.
“We found that half of the GCase in lysosomes from postmortem human GBA-PD [Parkinson’s disease] brains was present on the lysosomal surface and that this mislocalization depends on a pentapeptide motif in GCase used to target cytosolic protein for degradation by chaperone-mediated autophagy,” the researchers wrote.
Importantly, the team found that in the presence of alpha-synuclein, the mutated GCase caused nerve cells to die, but its wild-type version didn’t.
“This cell death was dependent on the presence of the CMA motif in GCase, indicating that the toxic interaction was dependent on [mutated] GCase inhibition of CMA,” they wrote.
In a Phase 2 clinical trial co-sponsored by Cure Parkinson’s (NCT02941822), ambroxol was found to reach the brain of patients with idiopathic Parkinson’s and safely increase GCase levels while reducing alpha-synuclein accumulation there. Scientists are planning a larger Phase 3 clinical trial to determine if ambroxol can slow the disease’s progression, the group stated on its webpage.