How Nerve Cells Damaged at Disease Onset Goal of EU Project
Andrii Vodolazhskyi/Shutterstock
An almost €2 million (about $2.3 million) EU-funded project is advancing the understanding of how damaged or abnormal cell parts are removed at the synapses, a process known as synapse-specific autophagy, and how defects in this mechanism contribute to neurodegenerative disorders such as Parkinson’s disease and Alzheimer’s.
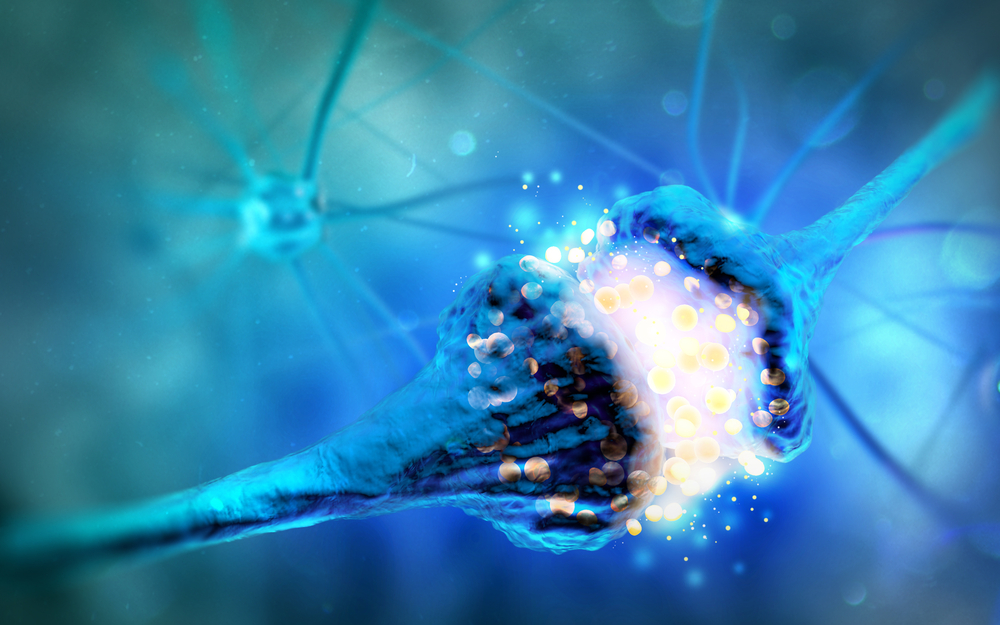
Synapses, the junctions between two nerve cells that allow them communicate, are affected early in the course of these disorders.
The ongoing and more than five-year project, “RobustSynapses, Maintaining synaptic function for a healthy brain: Membrane trafficking and autophagy in neurodegeneration,” is led by Patrik Verstreken, PhD, principal investigator and group leader at the VIB Center for Brain and Disease Research at KU Leuven, Belgium.
“The Robust Synapses project addressed one of the largest unmet medical needs — the fact that there are no cures for any of these major neurodegenerative conditions,” Verstreken said in a press release. “To meet this challenge, we wanted to zoom in on what is happening at the earliest stages of these diseases.”
Synapses are the gaps where electric nerve impulses are transmitted from one neuron to another. They allow communication between the brain and the rest of the body, and are involved in thought processes and memory formation. Neurodegenerative diseases like Parkinson’s are characterized by synaptic dysfunction, typically at their onset.
The researchers, who began by studying synapses in fruit flies using genome editing methods, discovered that specific mechanisms are necessary to eliminate damaged cell components, clearing cells of potentially harmful debris.
“If this does not happen, the synapses fail and cause problems,” Verstreken said.
Then, working with neurons generated from patients’ skin cells, the team confirmed that synapses fail to work properly when problems exist in the way that cellular debris at the synapse is removed, or synapse-specific autophagy.
Autophagy is an important process by which cells degrade or recycle components that are damaged or no longer needed. Cells use autophagy as a housekeeping “cleaning system” or to get rid of toxic materials, such as proteins damaged by disease and microbes. When autophagy is dysregulated and turns overactive, it can severely damage cells, including nerve cells, potentially causing them to die.
“One of our most exciting innovations was that we were able to develop tools that interfere with the defects induced by this process at synaptic contacts, including cognitive decline,” Verstreken said. “We are now pursuing this in the hope of developing real therapeutic interventions.”
Researchers also found that several genes coding for proteins associated with Parkinson’s — ATG5, ATG7, Synaptojanin, Parkin and LRRK2 — are involved in synapse-specific autophagy. In addition, EndophilinA — a protein involved in endocytosis, a cellular process whereby substances are brought into the cell — was found to be essential for synaptic autophagy.
According to the team, variations in the gene that codes for EndophilinA is a risk factor for Parkinson’s.
“[W]e found a way to interfere with the effects of ‘synaptic autophagy’. We can achieve this by manipulating proteins that are central to the process and that are also found to cause risk to Parkinson’s disease when mutated in patients,” Verstreken said. “We are now developing effective tools to achieve this, together with our industry partners.”
In another achievement, the researchers showed that more than 50% of the synaptic proteins, including alpha-synuclein (associated with Alzheimer’s) and tau (with Parkinson’s), can be broken down through a mechanism that involves Hsc70, an abundant synaptic chaperone protein. Of note, chaperones are proteins that help other proteins work properly.
These scientists also developed imaging methods allowing for high-resolution viewing of autophagosomes (a type of vesicle that engulfs damaged or abnormal cellular material during autophagy) at the synapses. And they created several fluorescent markers to better study other forms of autophagy and protein recycling at the synapses.
Their project’s ultimate goal is to find out how synapses function, so that clinicians might diagnose disorders at earlier stages and scientists develop more effective treatments.
“Given the large number of people suffering from neurodegeneration, the impact could be very sizeable,” Verstreken said.
The Robust Synapses project opened in January 2016, and is due to conclude on June 30, 2022.