Discovery of Key Feature of Alpha-synuclein May Lead to New Treatment Strategies for Parkinson’s
Written by |
Targeting certain regions of the alpha-synuclein protein could be a viable therapeutic strategy for Parkinson’s disease, a study suggests.
The study, “Two C-terminal sequence variations determine differential neurotoxicity between human and mouse α-synuclein,” was published in the journal Molecular Neurodegeneration.
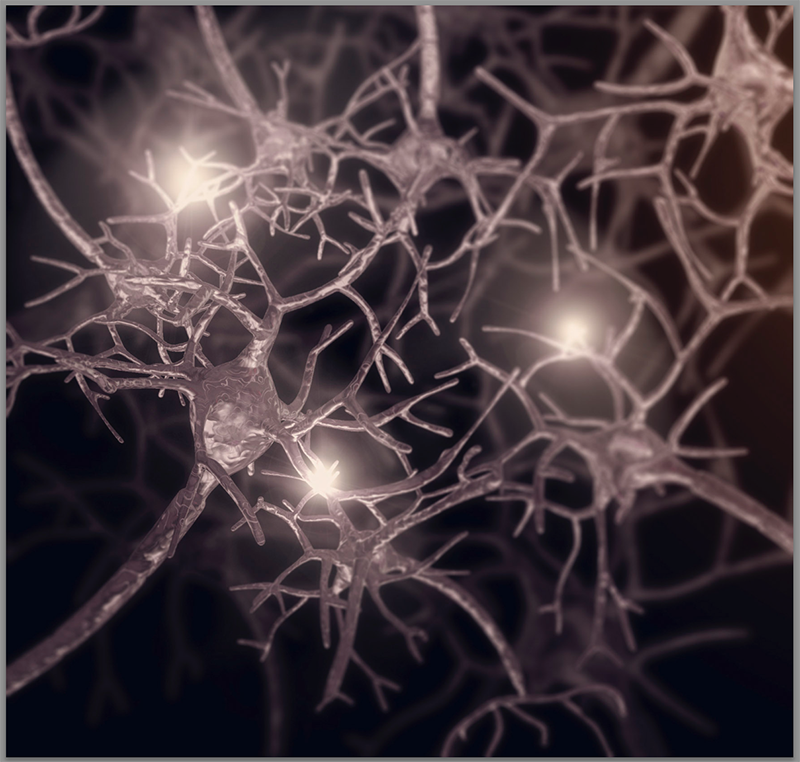
Parkinson’s disease is characterized by the accumulation of toxic aggregates of protein — particularly alpha-synuclein (aSyn) — in brain cells. Certain heritable mutations in the gene that provides instructions for making alpha-synuclein can directly cause Parkinson’s, though alpha-synuclein aggregates are widely thought to play a role in disease progression regardless of underlying genetics. Aggregates of alpha-synuclein are also involved in other neurological diseases, collectively termed synucleinopathies.
Given the central role of alpha-synuclein in Parkinson’s, stopping the protein from forming aggregates may be a viable strategy for treatment. However, developing treatments that can do this requires understanding exactly how alpha-synuclein aggregates form in the first place.
“A detailed understanding of molecular mechanisms by which aSyn forms neurotoxic aggregates is critical for developing therapies aimed at slowing neurodegeneration in the brains of patients with [Parkinson’s disease] and other synucleinopathy disorders,” the researchers wrote in the study.
The team at Purdue University and their colleagues set out to better understand how alpha-synuclein aggregates form by comparing human and mouse versions of the protein. While both humans and mice produce alpha-synuclein, the exact structure and sequence of the protein varies among different organisms — with some important biochemical consequences.
Specifically, in humans, a mutant form of alpha-synuclein called A53T is known to form aggregates and cause Parkinson’s. The mutated protein has an alteration in one of its amino acids, which are the building blocks of proteins; specifically, the amino acid threonine (T) is at the 53rd position, where there is normally an alanine (A).
Unlike human alpha-synuclein, the mouse version normally has a threonine at the 53rd position — however, the mouse version of the protein isn’t neurotoxic; it doesn’t form aggregates. This suggests that other differences between the two proteins are necessary for A53T to form toxic aggregates in humans.
To study this further, the researchers created chimeric versions of alpha-synuclein — essentially, they engineered versions of mouse alpha-synuclein where specific parts of the protein had been altered to resemble the sequence found in the human version of the protein, and vice versa. Then, they evaluated the cytotoxic (cell-killing) effects of these protein variants using cells in dishes.
One of the differences between human and mouse alpha-synuclein occurs at positions 121 and 122 in the protein chain; in humans, the amino acids at these locations are aspartic acid (D) and asparagine (N); in mice, they are glycine (G) and serine (S).
Mouse alpha-synuclein engineered to mimic the human protein at these locations was significantly more cytotoxic. Conversely, human alpha-synuclein with the A53T mutation was significantly less cytotoxic when it was engineered to have the mouse amino acids at these locations.
“Taken together, these findings suggest that residues D121 and N122 are important for the ability of [human] aSyn A53T to elicit … cell death,” the researchers wrote.
Experiments with the chimeric protein in rats showed similar results, supporting the role of these two locations in the aSyn protein for regulating cytotoxicity in living brains.
Additional experiments suggested that both the toxic and non-toxic versions of the protein formed overall aggregates to a similar degree. However, the extent of protein aggregation at the membranes of cells, specifically, was significantly higher for toxic versions of the protein. Toxic and non-toxic protein versions also differed in the extent to which they disrupted vesicles, which are small membrane-enclosed structures in cells.
“We show for the first time that this differential toxicity is associated with differences in aSyn-mediated vesicle disruption and aggregation at the membrane surface, rather than differences in aSyn fibrillization [aggregation] previously suggested to be important for modulating aSyn toxicity,” the researchers wrote.
“Most importantly, we provide evidence that these characteristics of the overtly toxic [human] aSyn A53T variant can be blunted, down to the same level of [mouse] aSyn, by modification of only 2 amino acid residues in positions 121 and 122 of the protein,” they added.
Since these positions are important for regulating the toxicity of the protein, targeting this protein region may be a therapeutic strategy. More research will be needed before such a strategy can be employed, since the role of these regions of aSyn in disease are “not well understood,” study co-author Chris Rochet, PhD, of Purdue University, said in a press release.
“We also don’t have a clear idea of the structure of that region of the protein,” Rochet said. “Based on what we know about the biochemistry of that region of the protein … it’s going to be difficult to target. … It’s possible, but there will be challenges.”


