Mechanism to weaken unused brain connections affected in Parkinson’s
New research findings may help in developing symptom-targeting treatments
Written by |
The brain weakens unused neural connections in the striatum, a region involved in motor control and decision-making, through a nitric oxide-dependent mechanism that appears to be disrupted in Parkinson’s disease, a study in mice suggests.
According to the researchers, these findings reveal some of the molecular mechanisms underlying the symptoms of Parkinson’s — and may help in developing treatments for the neurodegenerative disease.
“Now, the question is how restoring nitric oxide signaling might fix what goes wrong in the striatum of Parkinson’s disease patients,” D. James Surmeier, PhD, senior author of the study from Northwestern University Feinberg School of Medicine in Chicago, said in a university news story.
“The tools we have to monitor and manipulate brain circuits [have] rapidly expanded, deepening our understanding of how Parkinson’s disease affects the brain and giving us strategies for reversing the changes in circuitry that cause symptoms,” Surmeier said.
The study, “Ca2+-dependent phosphodiesterase 1 regulates the plasticity of striatal spiny projection neuron glutamatergic synapses,” was published in the journal Cell Reports.
Mouse study reveals molecular mechanisms underlying brain connections
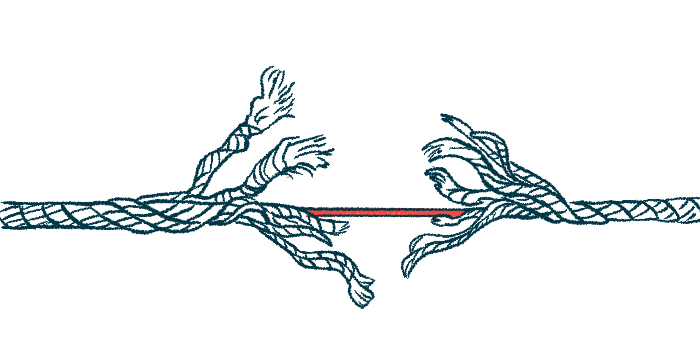
Long-term synaptic plasticity is a mechanism in the brain that allows neurons, or nerve cells, to strengthen or weaken their connections in synapses — the junctions between two neurons. This mechanism is key for learning new behaviors and forming habits over time.
In the striatum, spiny projection neurons, called SPNs, communicate at glutamatergic synapses, where they use the chemical glutamate to send signals. This mechanism, called nitric oxide-dependent long-term depression, or simply NO-LTD, depends on nitric oxide, a gas that acts as a signaling messenger in the brain.
“The [striatum] is one of the few places in the brain that has very high levels of the signaling molecules that respond to nitric oxide,” Surmeier said. “We wanted to get a better understanding of the role that form of plasticity played in controlling behavior.”
To that end, Surmeier and other scientists from both Northwestern and the Mount Sinai School of Medicine in New York teamed up to study these brain mechanisms.
The [striatum] is one of the few places in the brain that has very high levels of the signaling molecules that respond to nitric oxide. … We wanted to get a better understanding of the role that form of plasticity played in controlling behavior.
The researchers found that NO-LTD occurs mainly at quiescent synapses — those not currently in use. By weakening these unused neural connections, the brain can better refine its network.
NO-LTD involves calcium entering the neurons through protein channels. The flow activates phosphodiesterase 1, or PDE1, an enzyme that reduces the levels of a molecule called cyclic guanosine monophosphate (cGMP), which is important for nitric oxide signaling.
By reducing the levels of cGMP in neurons, PDE1 ensures that NO-LTD only takes place at unused neural connections, in contrast to parts of the neurons that are actively processing information.
“All of the commonly described forms of synaptic plasticity are dependent upon activity,” Surmeier said. “No one to our knowledge has described a form of synaptic plasticity that was enabled by inactivity at specific locations in a neuron.”
In a mouse model of Parkinson’s disease, NO-LTD was disrupted. The neurons failed to release enough nitric oxide, which is needed for NO-LTD to take place, “potentially contributing to a pathological [disease-related] distortion of the functional connectivity of SPNs and motor disability,” the researchers wrote.
However, restoring the balance of certain chemicals in the striatum, particularly dopamine and acetylcholine, triggered the release of nitric oxide and restored NO-LTD in a mouse model of Parkinson’s. This suggests that targeting this mechanism may ease the symptoms of Parkinson’s disease, according to the researchers.
The researchers’ work was funded in part by the JPB Foundation, the William N. and Bernice E. Bumpus Foundation, and the Simons Foundation. Support also came from grants from the National Institutes of Health.