My Symptoms Are Worsening, but Everyone Thinks I Look ‘Fine’
Written by |
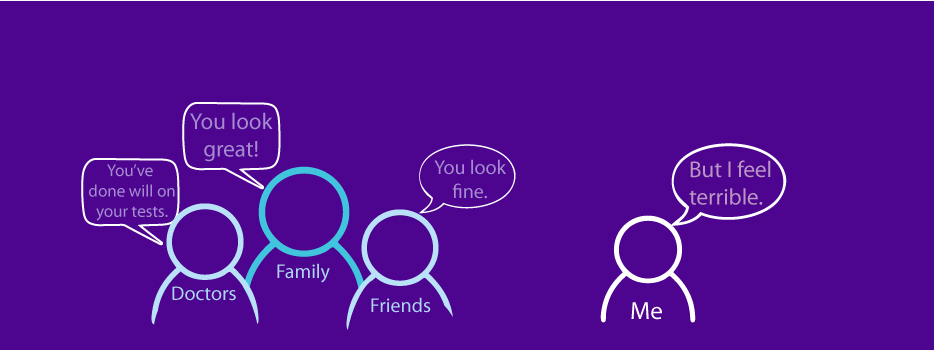
“I feel terrible, yet everyone thinks I look fine.” I’ve heard this sentiment expressed many times by folks with Parkinson’s disease.
So, why do we feel so bad?
I was diagnosed with Parkinson’s in 2015, and I am still so frustrated with trying to find relief from my symptoms. Just writing this column has been hard because I feel miserable, which makes it extremely difficult to remain positive.
My quality of life is deteriorating, mainly because of my nonmotor symptoms, which include overwhelming fatigue, speech and swallowing issues, apathy, depression, and a lack of motivation. Overall, I just feel terrible. Words like “weak,” “shaky,” “no self-confidence,” and “vulnerable” come to mind, but they don’t do justice to how horrible I feel.
My motor symptoms consist of bradykinesia, balance issues, and difficulty rolling over in bed. Other than exercise, I have yet to find anything else that can ease my symptoms. Commonly prescribed Parkinson’s medications, such as immediate-release carbidopa/levodopa (C/L), do not appear to provide me much relief from my motor symptoms.
Finding the right combinations and dosages of medications to help me maintain a good quality of life has been a frustrating effort. To make things worse, I feel as though my disease has been progressing quickly over the past year.
‘You look great!’
Everyone, doctors included, says I look great for someone who has had Parkinson’s for more than five years. My movement disorder specialist (MDS) is very frustrated with my case, as she doesn’t know how best to treat me. I am always telling her how awful I feel, and nothing seems to improve my quality of life.
My MDS suggested I add a new medication, Nourianz (istradefylline) to my C/L regimen, which is supposed to reduce my “off times.” My condition seemed to deteriorate even more after I started taking this new medication. My akathisia started to worsen about an hour before my next dose of C/L was scheduled.
I discontinued the Nourianz after about a month. The akathisia episodes, although not considered a side effect of Nourianz, stopped. I then tried Rytary, which replaces C/L, and the akathisia episodes returned with a vengeance. I discontinued Rytary and have now returned to taking my original medication.
Why does the MDS think I am doing well?
I perform well on the standard motor tests the MDS gives me. However, these tests only seem to focus on specific motor skills, and not every movement type that can be impaired due to bradykinesia.
For example, I can still walk at a fast pace, yet it can take me 10 minutes to put my clothes on in the morning. Sometimes, it takes me so long to put on a pair of socks, I exhaust myself and break out in a sweat. Yet, I can perform the finger-tapping, heel-stomping, and toe-tapping motor tests the MDS gives me with relative ease.
Is it all in my head?
At times, I wonder if my worsening symptoms are psychosomatic. Sometimes I feel as if it were all in my head. This is reinforced by everyone telling me I look great for someone with Parkinson’s, although I feel miserable.
In addition to my neurologists, I have also consulted with a naturopathic doctor. She was involved in the creation of an online tool called Patient-Reported Outcomes in Parkinson’s Disease (PRO-PD), a patient-centered, continuous measure of disease severity that correlates with quality of life. I repeat this test every few months.
The naturopath pointed out that my PRO-PD scores started to worsen last May. That is when I had my first elbow surgery, which prohibited me from exercising for several months. I had two more surgeries in December, further impacting my ability to consistently exercise. Add the isolation dictated by COVID-19, and you have a perfect storm. No wonder I feel terrible!
What I know
What is the bottom line? Can I feel as horrible as I do in contrast to what others see? Yes!
The following are reasons why:
- Parkinson’s causes many invisible, nonmotor symptoms that may make a person feel worse than the disease’s motor symptoms do.
- Just because a person with Parkinson’s doesn’t have any visible symptoms does not mean that the symptoms are “all in their head.”
- Exercise is critical to feeling good.
“Things are not always what they seem; the first appearance deceives many.” – Phaedrus
***
Note: Parkinson’s News Today is strictly a news and information website about the disease. It does not provide medical advice, diagnosis or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or another qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website. The opinions expressed in this column are not those of Parkinson’s News Today or its parent company, Bionews, and are intended to spark discussion about issues pertaining to Parkinson’s disease.



pamela thornton
I am frustrated by people trying to give me what they think would be helpful, such as a 'day out' which is actually useless as a 'cheery day', because I reach exhaustion point while I am out in public and in need of a bed and an hour's nap. The misery of standing, surrounded by people and feeling as if I am going to break in half at any minute, cannot be explained.
I hear you Pamela. Lately, I am trying to focus on my breathing to calm down my frustrations and it helps.
Paul White
I’m totally with you on that one. I’m currently in the bad books because I didn’t (couldn’t) join in the festivities.
No one gets it.
Christine
I understand your frustration. Usually I only go out when my meds are 'on', but if I stay out too long (say, stuck in a line in the grocery store) and I enter an 'off' time, it's like I can hardly stand anymore and my body explodes into violent tremors, I start sweating, and really can't concentrate. It's all I can do to pull out my credit card without dropping my wallet, pay, and get outta there! I feel like a ticking time bomb when I'm out in public. And, to be clear, that's just one example!
Exercise is my go-to as well, Jean, and I too have just started to practice focused breathing. It actually works remarkably well to get me through stressful moments. A friend of mine who also has PD, said something that really gives me hope, she said 'Parkinson's is not a one-way street' when I was bemoaning my health during Covid, and how it has impacted my exercise regime and how I felt I was going downhill quickly these past few months. I am hanging on to the hope that once I get back to my normal high range of exercise I can make some headway and feel strong again. I really hope you can too.
Christine, thank you for your comment and kind words of support... Ah yes, the grocery line, as I fumble in my purse for credit card, people behind me in line are getting impatient. I know the stressful experience you described... As for exercise, I am going to start slowly going back to Zoom Rock Steady Boxing classes within a few weeks (no punches with left arm due to elbow surgery). I too hope I can get back on track... Good luck to you.
Elizabeth Sanabria
I found your article very helpful and uplifting. I will continue with my exercise routine and look forward to some good years. Diagnosed two years.
thank you Elizabeth for your feedback. I still believe our best ally in fighting this disease is exercise. I wish you good health!
Thomas Perry
You have described my condition perfectly.
Thomas, Thank you for your comment. Yes, there are many of us in that boat. What is it about 'misery loves company' that gives us comfort? LOL
Grace
I have the same experiences as Christine my life has drastically since being diagnosed with Parkinson's disease. Jean I feel the same way too some times I wonder if it's all in my head. These days I don't even want to leave my house. Thanks Jean your articles are very uplifting they help me to realize I'm not alone in this battle and I'm not crazy either.
Grace
I hear you about not wanting to leave home, then you add Covid to the mix... Yikes. Thank you for your kind feedback. As I said to another commenter: "What is it about ‘misery loves company’ that gives us comfort? LOL"
Thomas Rutschman
Have you tried Mannitol? After 3 weeks I felt a lot better, with my face showing more emotions, and my arms swinging again when I walk. And I have had Parkinson's for ten years now.
hi thomas, that is wonderful! i tried mannitol for abut 4 months and saw no change in symptoms. unfortunately some remedies work for some and not others. i am still in search of what works for me! thank you for sharing!!
Craig
I was originally diagnosed with pd in 2003 at the age of thirty one. I find that exercise is what helps the most. I consider my job is to stay as healthy as possible. Michael J.Fox has said that no one dies from pd. They die with it.
Make sure that you lead a completely healthy lifestyle. Not to say that pd doesn’t kick my ass some days. But I will fight everyday. I am fortunate in that I have nothing else wrong with me other than pd Tim Hague a Parkinson’s patient in his book perseverance about his battle with pd says that pd is his best friend that he hates. I will let you figure out what that means. Change your schedule. When you feel bad working the computer. When the meds are working do things outdoors. Look into DBS. It works very well.
hi craig, thanks for your comments, Exercise has been part of my life since I was in my 20s. I am now 67. I used to be a dancer and a cyclist. i am thankful that i still have my drive and/or the ability to go on auto pilot with my exercise now that I have PD. I do need to get outdoors more. again, thank you for your suggestions
craig
Sounds like you will be fine. The one thing I would love to do is to run another marathon. I ran one in 1983 and always wanted to run another one. While I can still run a bit. I tend to drag my foot. It catches uneven road and I wind up face planted on the street. That got old quick I still haven’t totally given up this dream just need to figure it out. Remember to make friends with pd. It is my best friend who I absolutely hate God Bless
Craig, i drag my left foot sometimes and I have had a faceplant as a result. What has helped me is to focus on heel toe and being mindful of what I am doing. You are the second person who has said PD is there best friend that they hate. I have to think about that...
Fabio
Jean, I’m 44 and have early onset PD for 3 years. This last 3 years have been exactly the same kind of situation you described. However, things have changed recently, since a new doctor prescribed me a combination of Rasagiline (tablet) and a skin patch called Neupro (Rotigotine). I’m feeling the non-motor symptoms got about 80% better (even though the motor ones got a little worse...). But I’m much more motivated- I’m a musician, and not being able to play guitar properly anymore caused me severe depression and anger, but after this new medication, I felt motivated to focus on songwriting, I’m not feeling much chronic fatigue anymore and my mood is much better, I had my first happy moments since my diagnosis and became more hopeful again about the possibility of cure for our disease. If you haven’t tried these two drugs, maybe worth a shot, ask your doctor about it
hi fabio. thanks for sharing your experience. In addition to carbidopa/levodopa, I am on the Neupro 3mg patch and selegeline which is predecessor to rasagaline. what dose of neupro are you on? what motor symptoms worsened? We are all so different in our symptoms and react differently to the medications. I am happy you have found a combination that seems to work for you. i plan to talk to my neuro about increasing neupro dose and will look into rasagaline to replace selegeline
Marcy D Garb
I have found that 2mg of valium in addition to Sinemet helps with the small, full body tremors that make me feel anxious and frightened. I also take mannitol and am awaiting the results of the clinical trial at Hadassah Hospital that are expected to be published next month.
Marcy, we are all so different in our symptoms and what remedies work for us. Have you noticed a difference since taking Mannitol? Do you know where online the clinical trial results will be published? or can you subscribe somewhere for updates?
Sayeda
My husband has been diagnosed 4 years ago with PD.He has always been an intelligent,leader,go to guy ,resource on two legs ,quick ,affable and altruistic.
He now brings in pain ,feels afraid and cries not knowing why.
His neuro maintains he is doing well.
Each day is a challenge,but it is a gift. He is at my side,lucid when meds kick in.
I thank Almighty and pray for a miracle and His mercy.