Stool Calprotectin May Be Used as Marker of Bowel Inflammation in Parkinson’s Patients, Study Finds
The levels of calprotectin — a protein whose levels increase in response to tissue inflammation — in the stool may be used as a marker of bowel inflammation in patients with Parkinson’s disease, according to a recent study.
The results, “Fecal Calprotectin as a Marker of the Gut Immune System Activation Is Elevated in Parkinson’s Disease,” were published in Frontiers in Neuroscience.
A hallmark feature of Parkinson’s is the progressive degeneration of brain cells due to the accumulation of toxic clumps of alpha-synuclein, called Lewy bodies.
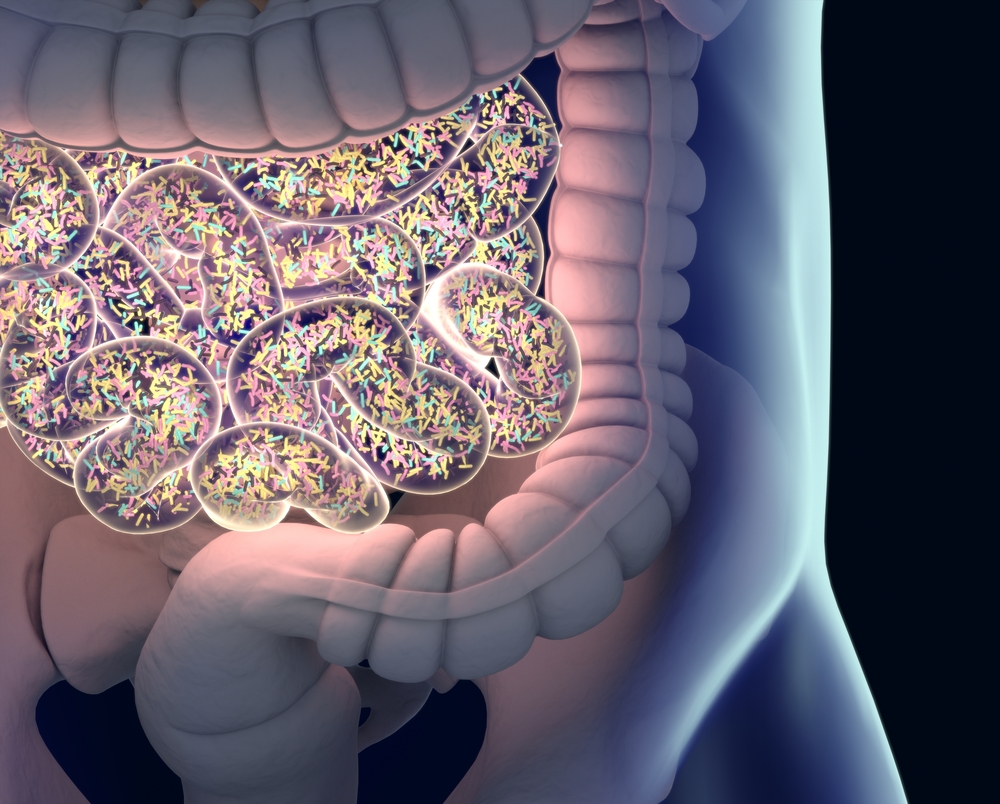
Some scientists believe Lewy bodies form in the enteric nervous system (ENS) — the network of nerves that innervate the gastrointestinal (GI) tract — then spread to the brain, where they gradually damage and destroy brain cells.
It also is thought that lesions in the ENS may be linked to bowel inflammation, dysmotility (impairment of GI tract muscles) and high intestinal permeability, all of which contribute to gastrointestinal symptoms of Parkinson’s disease, such as constipation.
In this study, researchers from Wrocław Medical University in Poland set out to explore the usefulness of calprotectin and zonulin — two proteins whose levels tend to increase in the presence of inflammation and immune system dysfunction — as markers of bowel inflammation and impaired intestinal permeability in patients with Parkinson’s disease.
To that end, they gathered stool samples from 35 patients with Parkinson’s disease who were either hospitalized or routinely followed at the Department of Neurology at Wrocław Medical University, and 20 healthy individuals (controls).
The levels of calprotectin and zonulin in the stool were measured by Enzyme-Linked Immunosorbent Assay (ELISA), a technique that allows researchers to measure the amount of a specific protein of interest using an enzymatic reaction. All study participants were asked to complete a short questionnaire regarding their GI symptoms.
Results showed the median levels of calprotectin found in the stools of patients with Parkinson’s disease were much higher compared to those found in the stools of healthy individuals (54.5 μg/g versus 9.7 μg/g), indicating the presence of bowel inflammation.
“Additionally, we evaluated the percentage of subjects with abnormal results considering the following age-dependent upper cut-off values of normal fecal calprotectin: 51 μg/g for subjects below 60 years of age, and 112 μg/g for subjects above 60 years. Abnormal fecal calprotectin level was found in 43% of all PD patients and in none of the control subjects,” the researchers stated.
Additionally, abnormal calprotectin levels were found more often among patients younger than 60 (50%) than among those who were older than 60 (39%).
No correlations were found between the levels of calprotectin found in the stool of patients and disease duration. Unlike calprotectin, no significant differences were found in the levels of zonulin between the two groups.
The most frequent GI symptoms patients reported in questionnaires included constipation (69%), feeling of incomplete evacuation (51%), bloating (51%), abdominal pain (20%), and changes in bowel movements (17%).
“The results of the present study confirm that [Parkinson’s disease] is characterized by the gut immune system activation,” the researchers said.
“The evaluation of fecal calprotectin level may be a useful tool to detect the signs of gut immune system activation present in a remarkable number of [Parkinson’s disease] patients, also in the early stage of the disease. Calprotectin may constitute a critical link between amyloid formation and neuroinflammatory cascades serving as a prospective diagnostic and therapeutic target,” they added.






