Finding Words to Describe Parkinson’s Pain
Written by |
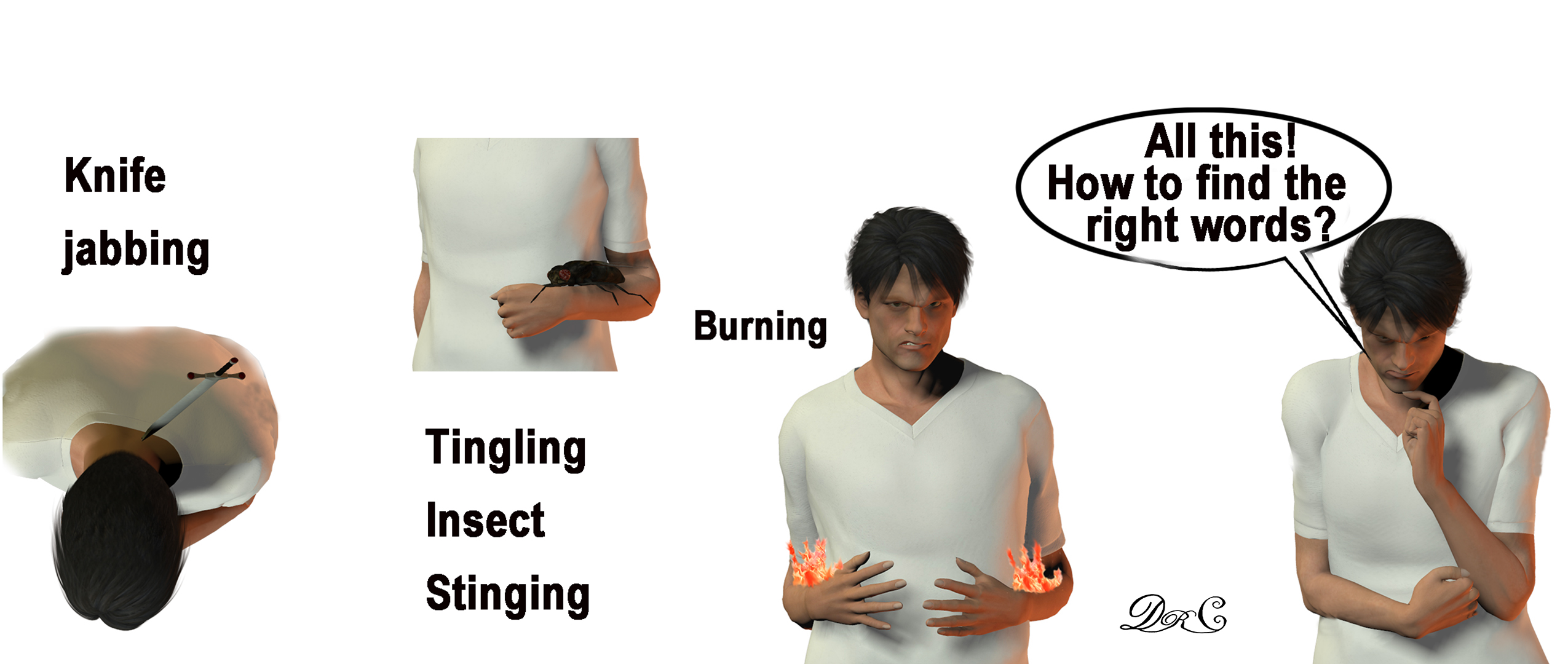
(Graphic by Dr. C)
Parkinson’s disease (PD) pain is unique, so finding words to describe it is difficult. Not all those with a diagnosis experience pain. But for some, like me, pain is the major, disabling symptom. It is important to find words that describe the pain experience as clearly as possible. There is no “grin and bear it,” nor is this “a pity party.” Instead, this is a search for accurate articulation of the pain experience to help maintain quality of life.
Pain may be an early symptom of PD, according to a study presented at the 2018 World Congress on Parkinson’s Disease and Related Disorders titled “Pain: A marker of prodromal Parkinsons disease?” The American Parkinson Disease Association published research that supports the connection of pain with Parkinson’s, suggesting that if the pain is relieved with dopaminergic medication and the patient has a pattern of painful sensations that correlate to “off” episodes, more credence can be given to the idea that the pain is PD-related.
The Parkinson’s Disease News Today forums are a place to connect with other patients, share tips and talk about the latest research. Check them out today!
PD pain can resemble pain from other disease processes, especially as the patient ages and faces a multitude of other pain-causing conditions such as arthritis, spine degeneration, poor muscular conditioning, and such. In my case, PD pain is distinguished by the following:
- The progression of body pain correlated with the progression of the disease over time.
- Levodopa, a dopaminergic therapy, successfully reduces the pain.
- The pain is worse during “off” periods.
My PD pain also has a particular characteristic: stinging (sometimes knife-jabbing), irritating tingling, burning, and muscle heaviness with increased pain on movement. This pain happens over large regions of the body and varies in severity. At its worst, it can last several days and reach level 7, inducing spontaneous tears.
PD with episodic chronic pain is disabling in several ways. First, high levels of pain obstruct clear thinking. Second, high levels of pain induce the fight-or-flight response, which interferes with emotion management. Third, the amount of energy necessary to manage it is very tiring (even more so in the face of the deep fatigue associated with PD). Chronic PD pain entails much more than body symptoms.
Parkinson’s pain is a total experience that touches thoughts, feelings, and relationships. Even when it’s a struggle, finding the words to describe pain experiences is imperative to maintaining quality of life in the face of a difficult diagnosis. Finding the right words helps one communicate the pain experience to care providers, family, and friends — a network of relationships that help form the foundation for quality of life. By communicating the pain, those close to me are more understanding of why I act the way I do, which helps to maintain those relationships.
Over the years, I have watched my PD progression. I have taken the warrior stance to do all I can to slow the progression. My hardest battle is with the total experience of chronic PD pain. Large blocks of time disappear into the fog of war. Over time, I have learned the importance of communicating about the pain daily, sometimes multiple times a day. My partner asks, “Where are you today?” I will say, “I’m at level 5,” followed by a quick mention of the most bothersome symptoms. In the past, I kept track of the pain levels throughout several months to create benchmarks. This is all part of finding the words to describe the Parkinson’s pain experience.
I have been a “communicator” most of my life, but it remains a struggle to find words that describe the unique character of PD pain. If you experience PD pain, please share your descriptors in the comments. Together we may find a common dialogue that will help others.
***
Note: Parkinson’s News Today is strictly a news and information website about the disease. It does not provide medical advice, diagnosis or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or another qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website. The opinions expressed in this column are not those of Parkinson’s News Today or its parent company, Bionews Services, and are intended to spark discussion about issues pertaining to Parkinson’s disease.





Rayilyn Lee Brown
trying to speak feels like strangulation and my whole body feels like a clenched fist when interacting with others..Rigor mortis without benefit of death.
ROSALIE MAUD
That description fits PD very well. The “Strangulation” to me is the extra mucus that collects, making me sound constantly nasal as if I have a cold. I try to cough, but to no avail.. My whole body does sometimes feel like a clenched fist, but not only when interacting with others. I have toes that are constantly curled under and make me walk like a “Weeble” but unlike Weebles I can, and frequently do fall down. This makes my whole body tighten up. Finally, “rigor mortis without the benefit of death” is getting more real, every day – my anxiety level is through the roof , and I wonder how much longer I will be able to function at all.
Dr. C
Thanks for adding your words to the dialog. It is great to see the language diversity. I like the "Weeble" analogy. Are those toys still around?
Roberta Cassell
You are describing me1 I have not been diagnosed yet but, I realise when I come home from where ever I go I am exhausted and then the burning and the nagging sciatica pain comes on and I can not sleep! I go through this almost everyday and tell myself I'm O k then, repeat it over and over and The pain in my knees makes me feel I will collapse going down hill! I change my shoes and I can expect pain ,body does not like change especially temperatures! What is the perspiration coming from ever sense the sartan drugs? my bowel is the biggest problem! Sorry my battery is low!
Randu
I completely understand the pain. My pain is more of a whole body muscle burn and painful joints. I can’t take Levadopa due to reaction. Marijuana is the only thing that helps and occasionally nicotine. Some days the pain wants to make me cry.
Dr. C
Hello Randu ~ Thank you for your comment on the column regarding pain with Parkinson's. I am also limited in the dosage of levo-dopa due to moderate allergy response. I am looking into medical cannabis as an additional therapy and hope to write about my experiences in the future. As with any medication or chemicals taken in to the body, there are risks and benefits. I hope my columns offer some suggestions for relief by adapting lifestyle changes whenever possible.
Dr. C.
Ryan
I’m terrified at all of this. I don’t have PD but starting to think my 44 year old wife does. Her dad was just diagnosed last year. During a visit three or four years back I noticed he was holding his right arm a lot in a guarded position, or his hand would start to move, and he would quickly run his hand through his hair or some other motion to control it. His facial expressions seemed slightly less active, hard to describe, like he would smile but something was slightly different about the muscle tone of his face. Then my mother in law said that he was “tossing and turning all night, sitting up in his sleep” and that she had to move to the couch a few times - that raised the alarm for me, because not long before I had read some information about PD’s early symptoms in some advertisement, just out of pure chance - but it all lined up - I didn’t say anything because my mother in law is a retired nurse and felt like I would be over stepping. A year later he was trying to toss a ball to my nephew and his arm wouldn’t make a throwing motion... not long after that he was given a “soft diagnosis” - started on PD medication and after improving, given his definite diagnosis last year. Well yesterday during a late lunch, I noticed my wife’s right hand flutter up and down at the wrist, not a smooth, rolling motion, but a jerky, jittery motion. I said “what’s going on there?” And she passed it off as low blood sugar or muscle strain, We had been up since 4 am and she hadn’t eaten anything until then and it was 1 PM. She did just cook and has strained her wrist before - but I felt like I was going to sink into the floor when I saw that. Now I’m watching her every move Ike a hawk and running on pure adrenaline - I am sick my stomach right now - shear terror. I know it’s not a death sentence and we will continue to have a great life together if she does have it, but I hurt for her so bad - I brought it up again later that afternoon and that she should see a doctor, if only for a checkup, but I am finding it hard to function right now and don’t know what to do.
Dr. C
Hi Ryan ~ This is Mrs. Dr. C. I understand what it is like to live with somebody who starts showing signs and symptoms that may be indicative of Parkinson's. A recent column by Dr. C. describes the various ways that Parkinson's may exhibit itself and how researchers and medical providers are starting to see it differently ("Putting Your Best Face Forward"). We faced that same terror when my husband was first being diagnosed. We believe the more you can understand the disease, the less the terror will be hopefully. It is always a difficult thing to manage one's concerns for loved ones. Both Dr. C. and I hope that you and your family are able to get some answers. Thank you for reading Dr. C's columns and for checking in with Parkinson's News Today other columns and research.
Emmie
I'm really sorry to hear about how difficult it is to process, that your wife might have it. Its a different experience for everyone as you may know already. My family member is in their mid 70's and in their 8 th year, since diagnosis. I have to keep him active and mobile indoors and outdoors, with all the necessary precautions, e.g. padded belt, walker, sponge helmet at night time, lots of cushioned furniture as falls become more likely, etc. He is still walking, though balance and energy can be an issue. There are anti inflammatory foods that also ease his pain. As hes gotten on the later side of 70, he suffers sciatica more recurrently. The higher dose CBD oil and other anti -inflammatory foods, e.g. a spoon of Tziki after every meal, also help his pain management. A lot of the therapy can be strengthened from sharing experiences and talking it out. My dad is so much less communicative on bad days, but on good days, he intermittently chatty. Please encourage her to keep active and buy an alarm reminder to know when to take her Levodopa doses. Please don't worry and reassure her as though she just needs to be more active.
Dr. C
Hi Emmie ~ Thank you for sharing your experiences with your dad. I like your comment about PD being "a different experience for everyone". I will be proving a possible explanation for why PD presents so differently in the population. This research and concept will be delivered in columns to be posted in September, October and November. Hope you can read those columns and follow along in my ideas.
Dr. C.
Deborah Webster
Your article is close to home for me. I experience a sensation like thousands of bees running up and down my body stinging continuously. Its so painful, I can't stay seated, or stand or lay without moving around trying to relieve the pain. The episodes last 6-8 hours with continuous pain. The last experience was on New Year's eve after I returned home from a party. I did not drink, take drugs, or do anything different other than talking with other guests. I was exhausted when I came home and that's when the stinging started. I started to panic because I knew what was going to happen.
In retrospect, I see that I was very exhausted and probably had a diminished amount of levodopa in me and was experiencing an OFF episode. At one point, I was trying to tell my husband what was going on and I used the term: "heebee jeebies." So he googled it and found that it was a description of what heroin addicts experience in detox.
I told the neurologist and she agreed that maybe that was a correct interpretation. I have told four different neurologists about this and they all say they never heard of it. My current neurologist suggested that it might be "akithisia" which is related to dyskinisia.
I am so thankful that you wrote this article because I don't feel alone and misunderstood - there are others who are experiencing something similar to me. I feel it was triggered by exhaustion and when I look back to other episodes, I see that they occurred after a lot of stimulation which might have paralled a drop in levodopa. You are correct in saying that our means of communication need to be better in order to express what we are feeling and maybe get some relief.
I wish you all the best. Thank you for giving me the opportunity to share this.
Terry Pollock
I've had tingling, burning pain for years, mostly in my feet and legs, now in my shoulders and arms. I was a mystery to my doctors for years before I was diagnosed with Parkinson's. I'm staying away from meds for Parkinson's because I'm already on so many for other problems. Is this the pain that other people have?
Gil Thelen
You post gets it exactly right. Difficult to describe but a total body, sapping experience that fogs the mind and induces torpor.
Michelle
The worst part is when your doctor's don't believe you and don't help you because PD "doesn't have" severe pain.
Nancy
Michelle, I agree and can validate your pain. I, too, have Parkinson’s and started having severe leg pain, mostly at night, a few months or so ago. This is exactly the response that I got from the PA at my appt. I would like to know if Dr. C has an approach we should use, how to communicate this with our doctor.
Dr. C
Hi Nancy ~ Thanks for the comment and invitation to give an answer to "how to communicate this with our doctor". My new book, "Possibilities with Parkinson's" puts down several ideas on pain in Parkinson's. Providers I've run into have had some very interesting comments -- "Parkinson's patients don't have pain" to "We know everything we need to know about Parkinson's" and so on. My advice is give your doctor a copy of the book so he/she can read that there are other Parkinson's patients that experience the same issues you face. And, if you find those golden words that turn your provider into a believer... email me! I'm still working on this issue!
Dr. C.
Edward Assad
My pain is everyday.When I take a dose of Levo,I get increased tremor and widespread pain in my right arm from hand,wrist,raw elbow nerve and finally shoulder.After about 20 minutes it calms down and I can function for an hour and a half which diminishes with each dose until my last dose at night which I only take so I'm able to go to sleep.I wake up 3 or 4 times each night trembling and aching.My right arm feels as if someone has twisted my wrist and is trying to lift my body off the ground from the shoulder.
I take 6 or 7 doses a day and get about 6 hours "on".The rest of the time I'm in stages of "off" and in extreme discomfort.When it's really bad I have to try and hold my arm still which is almost impossible.My doctor just nods when I inform him how bad it is and recommends wires coming out of my head.I'm 5 years in and see no one willing to try and help.I've
been to the Mayo clinic where they said take more levo.University of Florida offered the same unreasonable solution.It's like a bad joke and they don't hear anything you're telling them and offer nothing for the extreme pain and lack of any quality sleep.Makes me wish I had cancer or something that qualified me for pain or sleep aid.Not having a good nights sleep for years kind of wears on you if you know what I mean.
What happened to the right to try some of the existing drugs that are in clinical trials and just might help?There are anti-hypertension drugs and calcium channel blockers that try to protect neurons or help break down Tau.All I hear is no,no and more no's.
How long can one stand this pain without giving up.I understand how this can drive you to end the pain and the unresponsive medical experts.They seem intent on driving you to a final solution.I thought they swore an oath to help not ignore.
Good luck to all and hope some of you have a more compassionate medical community.
Dr. C
You may have noticed that the column did not get into the cornucopia of issues surrounding pain treatment. Also I am not a medical doctor. I can say that personally pain treatment has been a problem and I never have a day/night with zero pain. The reason I write about developing a personal "rehabilitation plan" is because I HAD TO DO SOMETHING about the pain. I had to find the best way to live in order to keep the pain as low as possible. It is a warrior's journey.
William Johnson
HAVE PAIN IN A LOT OF DIFFERENT PLACES. FOR INSTANCE, THE CRAMPS I GET EARLY IN THE MORNING ARE SO PAINFUL I FEEL LIKE CRYING BUT IF I GET UP AND START MOVING THEY GO AWAY. THE PAIN IN MY BACK IS ALWAYS THERE BECAUSE I HAD SURGERY A FUSION WITH HARDWARE WHICH WAS A BIG MISTAKE. NOW I AM HAVING PROBLEMS WITH MY NECK AND SHOULDER. THE THING THAT S DRIVING ME CRAZY WHICH BTW IS NOT PAINFUL IS MY FACE WHICH TIGHTENS UP ALL THE TIME
Dr. C
It is great to see all these responses to the pain column. I hope they continue. It gives us, the readers, an opportunity to see the words people use to describe their pain, and thus helps us in our struggle to describe our own pain. Thank you all!!
Gail
Thank you all for sharing your ways of naming the different kinds of pain one can experience, when using a rating chart of 0-10 doesn't capture the existential experience of parts of one's body hurting. For me, pain can be fluid or fixed (radiates throughout my hip and thigh, sharp, piercing as if it was a bite) or smoldering like a soft burn, sindging like from a flame. Or one can image electrocution, when the pain is "off the charts." Perhaps this is the "heebie jeebies a previous respondent discovered was associated with heroin.
Internal tremors in one's arms are like pulsations invisible to the eye but as if fluctuating, charging up the neuro pathways. One's legs can feel weighted, almost leaden, if one's meds. are ''off."
Dr. C
I hear what you are saying about a 1-10 chart, that it doesn't really get at the total pain experience. I think the usefulness of the chart is when I am in sync with my care giver about what the numbers mean. When we are both on the same page then the numbers communicate well. I like that "electrocution" analogy. I also get that on real bad days. Thanks so much for adding your voice. I think the pain experience with PD is not well understood. Maybe many voices can help make a difference.
Posy
For years before my diagnosis, My body felt heavy and achy. I had carpal tunnel ops, and worst of all, was having those awful “electrocution” sensations in my legs. (Was always told it was restless legs.)
Now, I am suffering nerve pain, just like sciatica, pretty consistently in my left leg, sometimes in my right, and Aching arms. I wasn’t warned by the consultant about PD related pain, and am finding it hard to cope.
Dr. C
Hi Posy ~ It has been my experience that people underestimate the degree that pain is involved in Parkinson's. It seems to prevalent among many Parkinson's patients and one that seems to be inadequately understood and undertreated. I appreciate your reading my columns and hope that you can share, and find, some answers within the BioNews family and forums.
Dr. C.
Irene Poland
Reading this, all the comments made me have all the answers I’ve been wondering about the pain I have that started for 2 months ago or so if it’s related to my PD. I just recently had blood test done to check if I have arthritis but the result came out negative. From everyone’s comments I can relate my pain to some of you. My body feels heavy and patches of pain in different parts of my arms and legs, especially my right arm that bothers me the most and radiates the pain to my right neck towards my head. Last night my son gave me edible that has THC and put me out to sleep and I woke up this morning with no pain.
Dr. C
Hi Irene ~ Thanks for adding your pain description to the conversation. There are multiple modalities out there to address pain and we will hopefully find more medical support for patients with PD who deal with the problems of pain. I appreciate your reading my columns and hope that you continue to check in with "Possibilities with Parkinson's" and the Parkinson's News Today community.
Dr. C.
Dani L.
My father had PD and the pain was unbearable to watch. I truly feel for you all. I am a RN and was reading this arrival as a way to describe a patients pain. I would like to inject that my dad used Rick Simpson Oil through a medical dispensary and he found excellent relief. He would put a tiny bit on a toothpick and the tremors would stop in 5-10 mins. I was very anti marijuana anything until I witnessed how it benefited my dad. God speed my friends.
Dr. C
Hi Dani ~ I appreciate your candor as a nurse and as a loved one of a PD patient. I am exploring the aspects of medical cannabis in treatment of PD pain. I have not written about this therapeutic modality because there are so many issues outside of the scope of medical treatment. It is, however, a subject for a future column.
Thanks for reading my columns on BioNews Parkinson's News Today. I hope you, as a medical professional, continue to consider this website as a well-grounded and well-rounded view from PD patients and their caregivers and loved ones as truly insight into the challenges. My goal is to combine scientifically based information alongside my personal journey with PD.
Dr. C.
Chuck
I stumbled across your article while researching papers on Glial Cells. I am part of a population being diagnosed with something called “Central Sensitization.”We feel your pain.” I did not know until today that Parkinson’s was a painful disorder, but now it seems obvious. You may want to google “Central Sensitization” just to see the similarities of symptoms.
Dr. C
Hi Chuck ~ Thanks for information -- I will definitely look to see what has been published. Parkinson's pain, in my opinion, is often misunderstood or undertreated. The basal ganglia is one of the areas involved in Parkinson's disease, according to some research I've read. But the dominant area involved is most likely in the connections between the prefrontal cortex and thalamus. I hope you can read some of my other columns that address the prefrontal cortex and thalamus connections -- referring to that process as the "Grand Central Station" and "Conductor" who help to moderate how pain manifests in Parkinson's. I will definitely check out your recommendation for "central sensitization".
Thanks for reading my columns on BioNews Parkinson's News Today. I hope you continue to check in to see what others are saying and doing to address the PD challenges.
Dr. C.
S H
Thank you for publishing this about the pain. I’m newly diagnosed with PD. Started on levodopa carbidopa about 2 months ago. Prior to starting on meds I had left sided weakness with occasional tremors in left hand. Some tightening from my left shoulder down my arm. Now I’m waking up in the middle of the night with excruciating pain down my right arm and hand. I told the doctor who suggested I might have carpal tunnel so I’m wearing a wrist brace at night which helps my concern is that my right arm has always been my good strong side. I have to wonder is this pain drug induced from the levodopa carbidopa? I feel I should wean off it versus trying new drugs. Thoughts?
Dr. C
Thanks for reading the column. There is mounting evidence that there is pain associated with early Parkinson's and there is research linking Parkinson's to Restless Leg Syndrome. I experience episodes of nighttime pain every few hours, every night. I am not a medical doctor so I cannot comment on medication. What I have found that if I get up, walk around for 5 minutes, stretch my muscles, the pain drops enough for me to return to sleep. You might want to reach out to a movement disorders clinic to discuss your situation further. They have a team of medical provider specialists who can probably best address how to manage your symptoms. You may have to look at a major medical facility to find a clinic but it is worth the search.
Thanks for reading my columns on BioNews Parkinson's News Today. I hope you continue to check in to see what others are saying and doing to address the challenges we all face.
Dr. C.
BB free
The pain is endless like Having your body in a vice. That constant tightening and throbbing so bad you can’t breathe. And the pain and pressure in the head is so bad you can’t think or talk. Muscle spasms not stop. I did the whole pain management thing. Waste of time and made me worse along with the criticism of being treated like a druggy having your pills counted and looked down upon like your a criminal with urine tests. I got tired of being in a wheelchair, unable to shower myself, make a sandwich. I turned to marijuana and using it as a vapor. It has changed everything. I’m so sad and angry that this is a natural remedy that could help so many and is being kept from the suffering. I refuse to suffer anymore and need to vapor daily for a quality of life. Thanks to taking matters in m own hands and using marijuana.
Roberta Cassell
You are describing me1 I have not been diagnosed yet but, I realise when I come home from where ever I go I am exhausted and then the burning and the nagging sciatica pain comes on and I can not sleep! I go through this almost everyday and tell myself I'm O k then, repeat it over and over and The pain in my knees makes me feel I will collapse going down hill! I change my shoes and I can expect pain ,body does not like change especially temperatures! What is the perspiration coming from ever sense the sartan drugs? my bowel is the biggest problem! Sorry my battery is low! Parkinsons is on both sides of family!
Dr. C
Hi Roberta ~ If you think your symptoms match the PD diagnosis, it is a good idea to see a movement disorder specialist because they know more about Parkinson's than other medical specialists. I appreciate your comments and taking the time to read my columns. You might want to check out "Putting Your Best Face Forward" for a discussion about how the age-old stereotype of Parkinsons is being changed.
Dr. C.
JONATHAN COLEMAN
Stabbing, Throbbing, Needles, Fire Ant Bites, Tingling, Pins, Twitching, Spasms(Sometimes in places that you wouldn't think could spasm), Bone Pain that aches, burns, cracks or feels like a long needle is being driving thru Bone "X", Arthritis, Carpal Tunnel, Hands and Feet are stiff, tight and cramped and have atrophied so much they are in a constant position as if unused, hurts to walk, lifting things is hard as hell, shaking so much that simple tasks become unbearable or impossible, laying down makes it worse because then the spasms and twitches actually make it so that you are literally being bounced up and down in bed frequently, but can't walk around house all day because, (1) tired as hell and, (2)hard to move let alone walk, (3) falling isn't fun, (4) would bother everyone. What sucks the most is that the pain doesn't stay still and it travels. One second it's a stabbing shoulder, knee, shin, thigh, toe(weird when your toes get stabbed), stomach(ohhhh god the stomach/abdomen pain, never stops but does get worse when it gets stabbed. Feels like someone plunging a knife into you and sometimes you wish because Hari-Kari may not be as bad as this for the rest of my life. The head pain is horrible, and the tremors you feel in your head as well, wtf is that? It's like something moving, or pulsating, but it's all over and I don't know of a blood vessel that big. The electric shock sensations are horrible to, zap zap. I didn't notice but has anyone had problems with their vision? Sometimes my eyes spasm or flutter and usually becomes hazy out of my right eye. The stomach/abdomen, back shoulders, thigh, ribs, muscles, feet and bone pain/spasm/twitches have become unbearable as of late. All of this started mildly when I was 16 to. Sadly I am undiagnosed but after reading this I am convinced that it is definitely PD, the finger flinches/twitches and muscle spasms when I was younger that all started this make a lot more sense now. I haven't heard anyone mention it but I think you guys should try Xanax, I take it as needed and only take a qtr of a 2mg at a time and try to keep it to half daily. It makes the symptoms less frequent and definitely deals with the anxiety/depression so much better. Without the Xanax I cannot function, am in so much pain its a 10, all of those symptoms I mentioned are constant and I find myself taking 7 showers a day just to have the heat wash over me. It would also be impossible for me to write this to because the brain fog is horrible and even trying to think takes forever. Trying to speak is absolutely insane, confusion is my best friend and pain is my lover. God Bless all of you and I hope you all get comfort or relief my friends. Thank you for your insights. Can someone please give me the info to a doctor or anyone that can help me and get me diagnosed. And please someone email me and talk, I really need someone to talk to that is going thru what I am and believes me and sees I am not just drug seeking, like all the doctors believe. Even when I tell them, I don't want any drugs I want answers so don't prescribe any. Some of these doctors are straight up jaded asshats.
Dr. C
Hi Jonathan, I can certainly understand the pain that you feel. You ask for help to find a provider who understands. I am not a medical doctor and cannot prescribe but I can say that it can be very tiresome for any patient to keep looking for the provider to support them through all of this. So much is not understood about PD, and especially pain associated with PD and the mental and emotional toll that takes on a person. Reaching out to a local PD support group might help you find providers in your area. The support groups are still trying to have virtual meetings these days so you can probably find one through American Parkinson's Disease Association if you look online.
Compassionate blessings,
Dr. C.
Paula Lamont
Hi Dr C, I have found your column to be a fascinating read. Reading it has answered a lot of questions, especially about the amount of pain experienced with PD. My husband has yet to be diagnosed but is waiting to be seen by a neurologist to see if he has PD. My husband has excruciating pain around his ribs, which he has had for over 20 years but is now unbearable. He’s had a slight tremor in his right arm which is getting worse and head shaking. If he stands up for longer than 10 minutes he feels as though he’s going to faint because his legs feel so weak. He’s lost so much muscle and strength and feels cold all the time. He has trouble speaking at times and feels as though his thoracic area feels squashed. He also feels that his vision has been affected. Do you think he may have signs of PD. Thankyou for reading my long post xx
Dr. C
Hi Paula ~ Thanks for reading the column. Pain in PD is a very discussed topic. In addition, I think pain in PD has an unusual relationship with a second dopamine center in the brain. I will be discussing in future columns to be published in September, October and November. I hope you get some support from the neurologist who might be able to identify his symptoms that can be treated. Not wishing anyone to have "PD" but knowing is better than not knowing. I can certainly relate to his concerns -- I have many of the same.
Dr. C.
Mona Chambers
As a care giver what is the best way that I can help my elderly mother, she's 85, describe her pain? Just today I asked, and she stated she couldn't describe it, and I was hopeful the article was going to give me some ideas. I haven't read all the comments either, as I'm sure responses will be resourceful as well.
We had her taking Cymbalta for her anxiety, and it was quite beneficial for treating the pain aspect, unfortunately, when we increased the dosage, it made her paranoid, and delusional, so we have to d/c it. Since doing so, she has complained of pain once again.
Dr. C
Hi Mona ~ Thanks for reading the column. You didn't say if your mom has PD or some other condition. If your mom has PD then maybe you can read the pain descriptions provided by people with PD who have commented. See if any of their descriptions resonates with her. In addition, I think pain in PD has an unusual relationship with a second dopamine center in the brain. I will be discussing in future columns to be published in September, October and November. I hope you can find some "words" for your mom.
Dr. C.
Stephen
I am a primary care physician with post-polio Sx (paraplegia, Lt>Rt). I addition to faster progression of weakness of the legs which I have noticed about 5 yrs ago, Dx of tremor was made in July, 2018. Tremor has been well controlled with carbidopa/l-dopa, with slowly increasing the dose (currently 10/100, 2 pills, four times daily (every 6 hours. Still, I feel uneasy when I move around due to balance problem.
More concerning is the new onset of following symptoms:
1. Acute chest pain. I went to ER but cardiac workup was negative on each cases (Aug, 2020 and Sept 2020). I noticed that chest pain (hard to describe - squeezing, burning, occasional stabbing?), and it comes every evening around 7 to 9 PM, couple of hours after supper.
2. Precipitous fatigue. Now, I drop to nap almost after supper. Although clinic is a rather heavy burden, 9 hours daily with 20-25 patients daily, I never have had this kind of fatigue before. It started about 2 month ago.
3. Difficult swallowing. Especially dry, solid - such as bread, or piece of meat. Even pills stock in throat, needing of copious amount of water to swallow.
4. Burning sensation slowly developing around neck and chin - comes and goes over a couple of hours.
These Sx are described as final stage of PD in some papers. I wonder this means that my PD course started running faster. If I have less than a year till the debilitation/death, I have start closing many things now - clinic and personal.
Dr. C
Hi Dr. Stephen, I'm not a medical doctor but my intent with the column is to research and describe what we can do to help slow down the progression. I think it is possible for us to mitigate the worst of the symptoms for a longer time. You certainly have the expertise to identify the problems. What I can offer in my columns is a shift in perspective on how to manage the disease. I hope my suggestions, reported sources of research and understanding of your concerns help. Your willingness to share your journey after reading my writing is appreciated. I hope to see your comments from the medical perspective on future columns.
Dr.C.
Matthew Faust
My shoulders are often stuck in a shoulder shrug position and they really burn and hurt because of it. Same thing with my face. Bright lights suck. I get banged up all the time in my sleep and i wake up yelling a lot. Meds dont work as well as they use to. PSP is suspected at this point. Not going to lie, it kinda sucks. Im only 41.
Rachel
I am not diagnosed by a neurologist yet, but is diagnosed by an ENT. I am only 37 Years old and it all started with a burning tongue went from doctor to doctor couldn't eat lost weight I was down to 88lbs. finally an ENT diagnosed me and told me to go to a neurologist (I am waiting for my appointment). I was taking Olanzapine long term for depression and anxiety. I believe I got PD from that medication but I do not know if I need to stop taking it.
Right now I am in horrible pain, my mouth, pain and limited opening and closing, my tongue burns like hot oil and gets worse when I try ice. tongue also hurts because it does not stop moving and getting bitten. my arms, my legs, my back, chest and so on. the type of pain is different with each part of the body, anything from painful tingling to burning to stubbing pain.
How can I treat this pain? how do I stop it if there are no medications?
what stage does it sounds I am at right now?
There is no history of PD in my family. I have autistic 3 years old twins I don't know if that could be related.
Please help
Mike LeBlanc
I have been at this for 19 years. I was diagnosed at 41 years of age and totally understand the "Rigamortis without the benefit of Death" . I have pain everyday especially at night. I don't sleep because my body is zapping inside, rigid and my limbs move to what my wife calls a dead bug position. Arms and legs go straight up to the ceiling and cannot be moved. My chest gets so rigid that it feels as if its going to squeeze my heart so that it will explode. My hips are now giving out to move to either side and I cannot move them back without help. This disease is cruel.