Impulsivity and Parkinson’s: The Itch that Must Be Scratched
Written by |
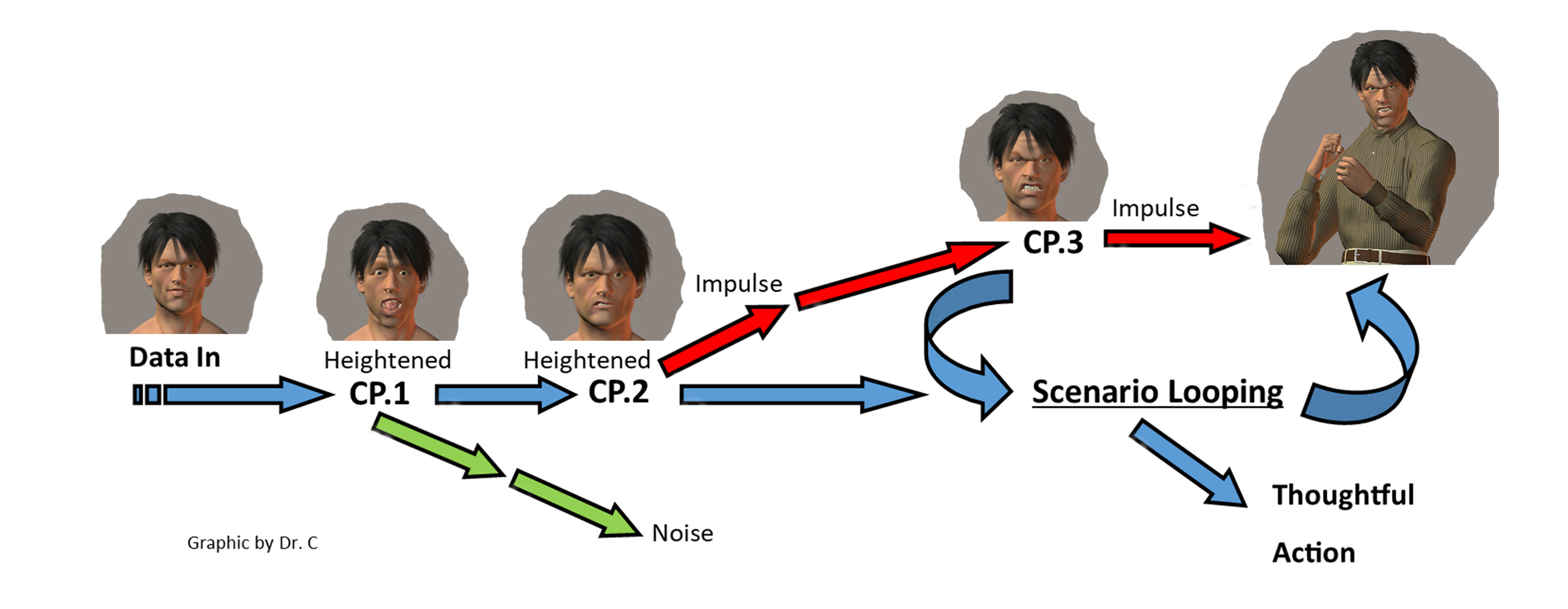
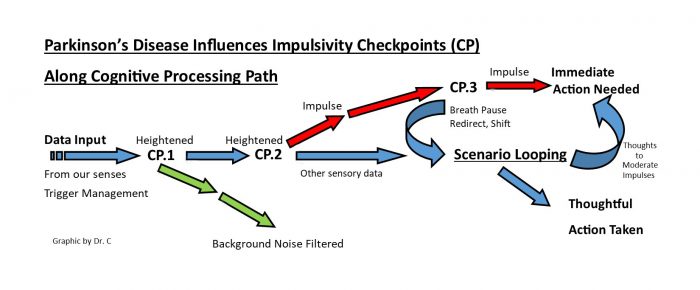
(Graphic by Dr. C)
Impulsivity is a symptom commonly associated with both Parkinson’s disease (PD) and some of the medications used to treat it.
Impulsivity involves acting on urges with little thought to the consequences — that seven-year itch that feels like it must be scratched — regardless of the problems that may arise. Impulsivity takes many forms. My previous columns about terror (exaggerated emotion) and irritability (the grouch) both speak to issues centered around impulsivity.
The cognitive pathways that involve impulsivity are simplified in the graphic below with the important checkpoints labeled as CP.1, CP.2, and CP.3. These checkpoints are where the impulse signals (sensory data) are heightened. The more heightened they become, the more difficult it is to alter their eventual destination of impulsive action.
PD creates problems at these three checkpoints and thus creates the false perception of heightened signal input and the false impression that it is the itch that must be scratched. Recognizing this is the first step in a rehab plan.
Interested in Parkinson’s Disease research? Sign up for our forums and join the conversation!
The study “Impulsivity and Parkinson’s disease: More than just disinhibition,” published in the Journal of the Neurological Sciences, provides an excellent discussion of the topic, as does the chapter “Impulse Control Disorders,” by Valerie Voon and Susan Fox, in the book “Parkinson’s Disease: Diagnosis and Clinical Management.” These authors point out that PD and the medications used to treat it directly affect the neural pathways used to regulate attention and impulse control. Any type of impulse can be affected.
Those with poor impulse control prior to PD onset were more likely to have more severe impulse control problems after PD onset. The contrary also is true. Those who practiced impulse control were less impacted. Our rehab to deal with impulsivity needs the daily practice of impulse control.
The above graphic is a representation of the cognitive pathways involved and the checkpoints we can become mindful of when developing a rehabilitation plan to address impulsivity. The arrows represent the flow of data or information into our brain (from left to right).
The first place we can begin our impulse control practice is with trigger management. In my first column for Parkinson’s News Today, I mentioned my problems with ice cream. It’s a love-hate relationship: I love it while my body hates it. Put a pint of Ben & Jerry’s in the fridge and I will devour it before the day is out. It’s the itch that must be scratched. The solution: Don’t put that ice cream in the fridge. This is called trigger management — the removal of the thing that triggers the impulse. This is step one in the rehab plan to deal with impulsivity.
Step two is impulse checkpoint awareness and adjustment. There are three checkpoints, and all three affect the perception of information coming into our brains. Thus, they affect impulsivity.
Checkpoint one is a background noise filter. Our brains don’t consciously process everything that the senses pick up. Think of all the noises, sights, and smells that are around you every day. Normally, you do not attend to them all and do not remember them all. Your brain filters them.
I think that PD (and medications) affect this filter. For me, subtle sensory stimuli have become heightened, and normal stimuli can take on an exaggerated importance. Sounds from a creaking house seem louder and more threatening, and shadows seen through the corner of my eye seem like someone moving. The startle response in me can become triggered as if a gun went off nearby.
This startle information is sent to checkpoint two and given emotive character, or a perception of danger in the home. Now the fight-flight response is added to the character of the signal.
The data signal has been heightened twice before getting to the last intervention checkpoint prior to becoming impulsive action. This is checkpoint three and it is tied to scenario looping. Step three in the rehab plan involves applying scenario looping for thought inputs that can moderate the need to scratch that itch. This can be done through various brain training practices.
My next column will address brain training practices in connection with impulsivity. What issues have you had with impulse control and what is your strategy to deal with them?
***
Note: Parkinson’s News Today is strictly a news and information website about the disease. It does not provide medical advice, diagnosis or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or another qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website. The opinions expressed in this column are not those of Parkinson’s News Today or its parent company, Bionews Services, and are intended to spark discussion about issues pertaining to Parkinson’s disease.






Francine Cole
Great information Dr C.
Joyce
Thanks for the information. My husband’s literal itch is triggered when he lies down. How does he remove lying down? What else can we done?
Dr. C
Hi Joyce ~ Thanks for your comment. There isn't enough information in your comment for me to understand what is going on. Can you expand on this a bit? I don't know if I am in a position to offer any advice based on your initial comment.
Dr. C.
Shirley
Is there anything you can take or do to stop the itching or what do you do to change the behavior
Shirley Stephens
What can be done to help the itching? A way to correct the impulse.
Shirley Stephens
Is there anything that can be done to alleviate the. Itch
Dr. C
Hi Shirley ~ Hope you can read along in the columns about the "conductor/exercise training" that I suggest will help with managing the impulsivity.
Dr. C.