University Awarded Prestigious Grant for Deep Brain Stimulation in Parkinson’s Research
Researchers at the University of Alabama at Birmingham (UAB) were awarded a five-year $7.3 million grant from the National Institutes of Health (NIH) to evaluate new technology that could potentially improve outcomes from deep brain stimulation (DBS) in Parkinson’s disease patients.
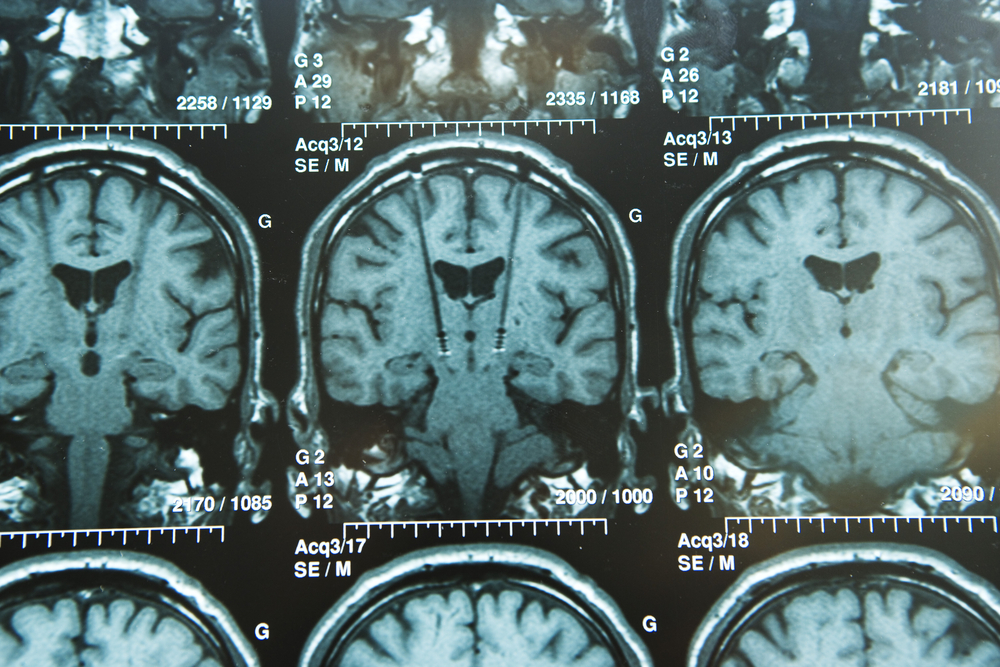
The research grant is part of the White House BRAIN Initiative (Brain Research through Advancing Innovative Neurotechnologies), a collaborative effort that will enable UAB investigators to assess next-gen technology that can direct current in specific directions in the brain, allowing a more precise DBS treatment adjustment. This approach can potentially enhance treatment outcomes and minimize side effects.
DBS is a neuromodulation therapy that uses electrical current to improve slowness, muscle stiffness, tremor, and other disabling symptoms of movement disorders. The technology will allow researchers to adjust treatment by measuring brain rhythms triggered by DBS during surgery and then testing these brain rhythms to see if they can serve as road maps in each individual to optimize stimulation as quickly as possible.
“One of the difficulties in current DBS technology is that the electrical stimulus goes out in all directions, like a radio wave from a broadcast tower,” Dr. Harrison Walker, MD, primary investigator of the study and an associate professor in the Department of Neurology, said in a press release.
“Based on previous studies in our laboratory, we believe that we can use this new electrode design to tailor the shape of the DBS electrical field in individuals and get better results with fewer side effects,” he said.
The research team will also study whether there are particular patterns of cortical activation triggered by the DBS pulse that can predict the best combination of DBS contacts for clinical therapy.
Researchers will also assess the potential value of these biomarkers in the refinement of the DBS electrode during surgery and in the improvement of long trial-and-error processes of adjusting stimulators in the clinic.
After surgery, patients are to participate in a crossover study comparing outcomes with and without directional stimulation. At the end of the crossover study, researchers will measure motor, cognitive, and behavioral outcomes. Participants will be asked which treatment strategy they preferred according to their chosen quality-of-life measurements and changes in symptoms.
“In addition to rigorously evaluating directional stimulation, this trial should allow us to identify physiological measures that could eventually be used to adjust DBS settings in real time based on the needs of the patient in daily life,” Walker said.
“Additionally, this work could serve as a foundation to guide neuromodulation strategies for other movement disorders and for emerging indications such as epilepsy, obsessive compulsive disorder, major depression and other disorders,” he added.