Vitamin A Supplement Fails to Protect or Treat Rats in Parkinson’s Disease Model, Study Says
Vitamin A, or retinol, given as an oral supplement did not prevent the loss of dopamine-producing neurons or lessen motor deficits in a rat model of Parkinson’s, a study reports.
Results also showed that retinol lowered levels of inflammatory markers in the blood and did not cause oxidative damage in the liver, but its use changed in potentially harmful ways the activity of inflammatory cells in the brain of rats without Parkinson’s.
The research, “The effects of retinol oral supplementation in 6-hydroxydopamine dopaminergic denervation model in Wistar rats,” appeared in the journal Neurochemistry International.
In the central nervous system, retinol (a type of vitamin A) plays diverse roles, including neuronal differentiation during embryonic development and long-lasting communication between neurons (nerve cells) in a key brain area involved in memory, the hippocampus.
Although in vitro (in the laboratory) and in vivo (with animal models) studies have reported that retinol has antioxidant and cell protective effects, and suggested a link between vitamin A deficiency and cognitive decline in Alzheimer’s, the use of retinol in prevent neurodegenerative disorders has not been fully explored.
The Parkinson’s Disease News Today forums are a place to connect with other patients, share tips and talk about the latest research. Check them out today!
To assess dietary retinol in Parkinson’s, researchers used a rat model in which a neurotoxin called 6-hydroxydopamine (6-OHDA) is injected into the brain’s substantia nigra, inducing the death of dopamine-producing nerve cells. This mimics hallmark changes in advanced Parkinson’s, leading to similar motor deficits.
The animals were given a form of retinol (retinyl palmitate, 3000 IU/kg per day, which is equivalent to 900 μg/day in an adult) orally over 28 days, followed by 6-OHDA injection. Their motor coordination, degree of neuroinflammation, and the content of dopaminergic neurons in the substantia nigra were then assessed.
As retinol supplements are also reported to have toxic effects, the scientists also looked systemic inflammation, liver toxicity, oxidative stress, and mutagenicity, or a toxic agent’s ability to cause mutations.
Data first showed no changes in 6-OHDA-induced oxidative stress or mutagenicity in the liver – the major organ in retinol storage – in treated animals. Retinol use also prevented a rise in blood levels of TNF-alpha and interleukin (IL)-1beta – two key mediators in the inflammatory response – in rats with Parkinson’s.
But retinol use did not protect against the loss of dopaminergic neurons and did not significantly ease motor deficits in the animal model. The rats’ motor function was tested 15 days after 6-OHDA injections.
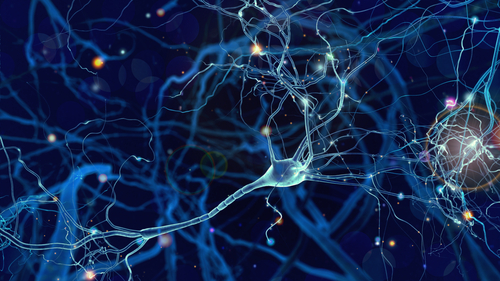
In the substantia nigra, retinol administration was able to prevent the activation of microglia — key immune cells in the brain — but not of astrocytes, cells whose various functions include a role in the formation of the blood-brain barrier and response to injury.
However, rats without Parkinson’s-like disease (no 6-OHDA injections) and treated with retinol showed increased astrocyte activation. These cells can both work with and inhibit microglia, to boost or block neuroinflammation, the researchers said.
“These results, altogether, suggest that oral supplementation with retinol does not protect against dopaminergic toxicity in the [substantia nigra] and may disturb astrocytes and microglia functional homeostasis,” they concluded.