Stem Cell-derived Therapy Eases Motor Deficits in Parkinson’s Model
Injected treatment brings BDNF, which promotes neurons, into rats' brains
Written by |
A transplant of stem cell-derived nerve cells engineered to produce a signaling factor that promotes nerve health was shown to lessen motor deficits and increase dopamine activity in a rat model of Parkinson’s disease.
The signaling factor, BDNF, is seen as a potentially effective treatment for Parkinson’s. While it cannot, on its own, pass through the brain-blood barrier, the membrane protecting the brain from possible insults in circulating blood, stem cells can be modified to carry BDNF, the researchers noted.
Their study, “BDNF-modified human umbilical cord mesenchymal stem cells-derived dopaminergic-like neurons improve rotation behavior of Parkinson’s disease rats through neuroprotection and anti-neuroinflammation,” was published in Molecular and Cellular Neuroscience.
Parkinson’s is caused by the death and dysfunction of neurons (nerve cells) in the brain that make a chemical messenger called dopamine.
Stem cells are specialized cells that are able to grow and differentiate into other types of cells. Some stem cells can be grown into dopamine-producing neurons, and in recent years as understanding of these cells has advanced, researchers have been exploring whether stem cell-derived neurons could be used as a therapeutic tool for Parkinson’s.
Study into the possibility of a stem cell therapy for Parkinson’s
In this study, scientists in China used stem cells derived from human umbilical cords to generate dopamine-producing neurons, referred to as dopaminergic-like neurons or DLNs. For some of these DLNs, the researchers used genetic engineering techniques to increase the production of BDNF, a signaling molecule that promotes neuronal survival and growth.
After performing a battery of tests to characterize these stem cell-derived neurons, the researchers explored their therapeutic potential by implanting these DLNs into brains of rats in an animal model of Parkinson’s disease. The model was induced by injecting a toxic chemical into a specific region of the brain (the striatum) to destroy dopamine-producing neurons.
Rats treated with DLNs had higher numbers of dopamine-producing neurons and higher levels of dopamine in their brains, results showed. The effect was more potent with DLNs engineered to make BDNF, as compared with unaltered DLNs or stem cells. Adding an antibody that blocks the protein receptor for BDNF also blunted the response.
Treatment with the BDNF-producing DLNs also reduced markers of cell death. Other biochemical analyses suggested it increased markers of nerve cell health and reduced the inflammatory activity of brain cells called astrocytes and microglia.
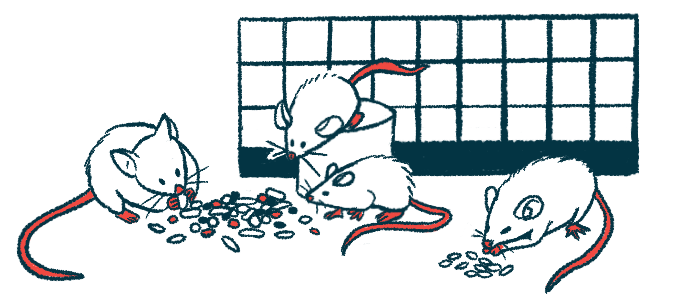
The rats were also assessed via the apomorphine rotation test, a measure of motor impairment conducted by injecting a chemical into the rats’ brains. In typical Parkinson’s rats, this injection prompts the rats to spin in circles, and the rate of spins increases as the disease progresses over time.
In Parkinson’s rats treated with DLNs, however, the number of spins decreased over time. The effect was most pronounced with DLNs engineered to produce BDNF.
“Our results suggest that BDNF-modified [DLN] transplantation significantly ameliorated deficits in rotation of the [Parkinson’s] rats,” the researchers concluded, adding that these effects are likely mediated “through neuroprotection and anti-neuroinflammation.”
The team noted that all analyses in this study were relatively short-term, highlighting a need for further investigations of the long-term effects of these types of cell therapy.