Parkinson’s Researcher Awarded $1M Grant to Study Diabetes Drug
Researchers at the Department of Neurological Surgery at Case Western Reserve University School of Medicine and University Hospitals Case Medical Center recently received a $1 million grant to investigate the effectiveness of a diabetes drug for treating Parkinson’s disease.
According to a press release from the UH Case, Barry J. Hoffer, adjunct professor of neurosurgery at Case Western Reserve and a member of the Department of Neurosurgery at UH Case, received the three-year, $1 million National Institutes of Health (NIH) grant to continue his research on the role of gliptins in Parkinson’s disease. The grant was one of several multi-million awards to Case researchers.
Gliptins are a class of relatively new drugs with the ability to regulate blood glucose levels, and are currently approved for type 2 diabetes. Following evidence that gliptins also show neuroprotective effects in Alzheimer’s disease, researchers studying Parkinson’s started demonstrating interest in this class of drugs a couple of years ago.
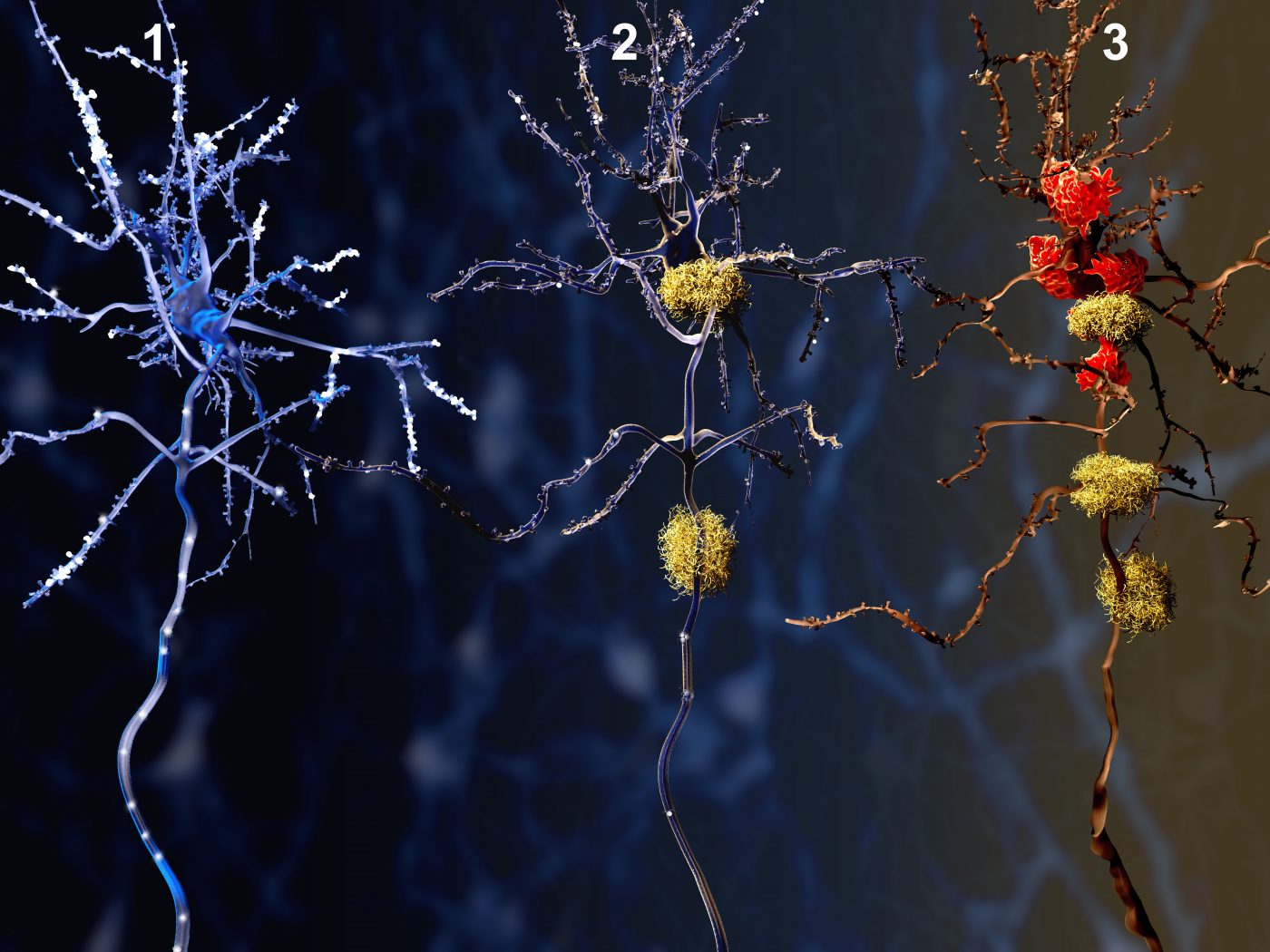
By increasing the level of incretins — a group of metabolic hormones involved in the lowering of blood glucose — gliptins also hold promise to effectively decrease Parkinson’s symptoms. Incretins, which readily enter the brain via systemic circulation, have receptors present in neurons. Previous work in cell culture models — in which Dr. Hoffer was also involved — revealed that when activated, incretin receptors promote growth and mediate protection of neurons from toxic insults relevant for Parkinson’s disease. Moreover, gliptins were also found to reduce Parkinson’s symptoms in a rat model.
The new grant will allow Dr. Hoffer to continue his work in mouse models, furthering the evaluation of gliptins as a new treatment strategy for Parkinson’s disease. Since 50%-80% of Parkinson’s patients also have glucose tolerance issues, gliptins may serve concurrently to improve both metabolic and neuronal dysfunction.
The research on gliptins for Parkinson’s disorder has a major advantage: several gliptin drugs are already available on the market. Repositioning the drugs for Parkinson’s is a process that is far shorter and cheaper than the development of a novel substance, as data on pharmacokinetics (absorption, distribution, metabolism, and excretion) and safety is already available from previous clinical trials. The process also reduces the cost of developing a drug by up to 40 percent.
“Currently, there is no cure for Parkinson’s, and while medications can dampen symptoms, the drugs become less effective over time. Our research is part of an effort to find new strategies to protect nerve cells involved and to at least slow, if not stop, the degenerative process,” Dr. Hoffer said.
Dr. Hoffer will be working closely with Yu (Agnes) Luo, PhD, and Xin Qi, PhD, from the Department of Physiology at Case Western Reserve University School of Medicine, and Michael Zigmond, PhD, at the University of Pittsburgh, on the project.
According to the press release, Dr. Luo also received a five-year, $1.7 million NIH grant to investigate new methods of regenerating stem cells, already present in the brain, to promote healing following a stroke. Dr. Eli Bar, an assistant professor of neurosurgery at Case Western Reserve, was also awarded a five-year, $1.8 million NIH grant for investigating why brain tumor stem cells are so resistant to conventional therapy. The grants further uphold the institute’s ranking among the top 25 U.S. research-oriented medical schools.






