New screening system helps to ID pesticides linked to Parkinson’s
Trifluralin, a driver of nerve cell toxicity, worse with other pesticides
Written by |
Researchers have identified certain pesticides used in agricultural settings that were linked to Parkinson’s disease risk among people living in California — and that were toxic to nerve cells in laboratory studies.
Particularly, a pesticide called trifluralin was a significant driver of nerve cell toxicity, an effect that was stronger when the chemical was combined with other pesticides.
The scientists believe their approach of evaluating pesticides from both a field- and lab-based perspective “may prove useful to mechanistically dissect pesticide exposures implicated in [Parkinson’s] risk and guide agricultural policy.”
The study, “A pesticide and iPSC dopaminergic neuron screen identifies and classifies Parkinson-relevant pesticides,” was published in Nature Communications.
Screening uses geographic data, lab results
Parkinson’s disease is a complex neurodegenerative disorder characterized by the progressive loss of certain nerve cells, called dopaminergic neurons, that produce the dopamine signaling chemical.
It’s thought to arise from a combination of genetic and environmental risk factors. Among environmental factors, long-term pesticide exposure has emerged as a leading contributor to Parkinson’s onset and progression.
Pesticides are commonly used by farmers to protect their crops from unwanted pests. Still, the potential toxic effects of a majority of commonly used agricultural pesticides and their impacts on dopaminergic neurons have not been explored.
“While pesticides are important components of modern commercial agriculture that help maximize food production, most pesticides that are applied at industrial scales have not been adequately assessed for their potential role in [Parkinson’s], let alone for their mechanisms of action,” the researchers wrote.
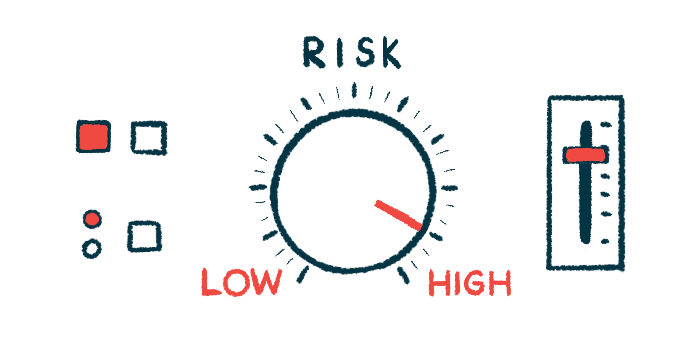
Now, these researchers developed a screening system that combines epidemiological data and lab-based studies to look for pesticides with a possible link to Parkinson’s.
First, they analyzed agricultural records in California to identify pesticides that were used in significant amounts near the residence or workplace of individuals included in the Parkinson’s Environment and Genes (PEG) study.
The analysis included 829 people with Parkinson’s disease and 824 healthy individuals, and their possible exposure to pesticides from 1974 to 2017.
On average, the Parkinson’s patients were more likely to live and work near agricultural facilities that used more pesticides than were the healthy people. Throughout the entire exposure period, those in the patient group were exposed to an average of 50 pesticides each at home and work. Meanwhile, the healthy individuals were exposed to an average of 45 at home and 38 at work.
Among 288 pesticides used in the vicinity of at least 25 study participants each, 53 were found to be statistically associated with Parkinson’s disease.
The researchers noted that 43 of them are considered “bad actors” by the Pesticide Action Network. This means they have been marked as toxic to humans in some way.
Scientist stress no causal link found for pesticides and Parkinson’s
Next, 39 of these pesticides were incubated in the lab with dopaminergic neurons derived from Parkinson’s disease patients, to identify their potential neurotoxic effects.
Ultimately, 10 pesticides were found to be directly toxic to nerve cells. Some of them previously had been linked to Parkinson’s, but others were newly identified, according to the authors.
Half, or five of the 10 pesticides, appeared to be specifically toxic to nerve cells, that is, they did not show similar toxicity in another cell type at the tested concentration.
In commercial agricultural, many pesticides are not used in isolation but are regularly combined and applied on the same field as others in the same season. Thus, the researchers next aimed to investigate how combined used of pesticides might influence their toxicity.
In fact, the researchers found that individuals’ real-world exposure to the 10 identified neurotoxic pesticides were highly correlated with exposure to a range of other pesticides that were not found to be toxic or were not tested.
A particular cluster of pesticides often used together were further analyzed for their potential effects on dopaminergic neurons. Many pesticides found in this group are related to cotton farming, and thus it was dubbed the “cotton cluster.”
Results showed that combinations of pesticides involving trifluralin led to the most substantial nerve cell death.
For example, trifluralin on its own led to a 32% loss of dopaminergic cells, while another pesticide called tribufos led to an 8% loss. Together, they produced a 65% reduction in cells.
Trifluralin, an herbicide used to control grass and weed growth, has been previously implicated in Parkinson’s, “making this a compelling pesticide for more in depth mechanistic investigation,” the researchers wrote.
Additional experiments in dopaminergic neuron cultures revealed that trifluralin might exert its toxic effects by causing dysfunction of mitochondria, the organelles needed for cellular energy production.
A similar approach should be taken to explore the mechanisms of other top-hit pesticides, according to the authors.
The team emphasized that they “view population-based screening as a first step to prioritize agents for more in-depth research.” The findings do not confirm a causal role for any pesticide in Parkinson’s, but “nor does it absolve those which failed to screen positive for a role” in the disease, they wrote.